Diagnostic errors are an inevitable aspect of modern medicine.
The human body’s complexity, combined with the subtle ways diseases present themselves, creates inherent challenges. Approximately 5.7% of all emergency department visits involve a diagnostic error, despite the expertise and dedication of medical professionals.
This stems from medicine’s fundamental complexity.
Countless symptoms overlap between different conditions. Rare diseases masquerade as common ones. Patients describe their experiences differently. Laboratory values fall into gray zones.
The sheer volume of medical knowledge, doubling every 73 days, exceeds what any human can master. This knowledge explosion, combined with other diagnostic complexities, creates natural limitations that no amount of training or experience can eliminate.
AI offers a complementary approach to these inevitable challenges.
By analyzing patterns across millions of patient records, these systems detect subtle disease signatures that conventional methods might miss. AI can identify early-stage cancer from imaging that appears normal to radiologists, recognize cardiovascular disease from ECG patterns before symptoms develop, and highlight medication interactions that might otherwise go unnoticed.
Healthcare organizations seeking to implement these AI tools need specialized guidance from AI healthcare consultants, who connect medical teams with properly validated diagnostic systems that enhance clinical capabilities.
By ensuring AI solutions amplify physician expertise rather than replace it, these consultants help address the inherent diagnostic challenges all healthcare providers face.
Throughout this article, we’ll examine how AI impacts diagnostic accuracy through documented outcomes.
You’ll discover how these technologies identify diseases months before conventional detection methods, learn how leading institutions have improved diagnostic precision, and understand the practical steps medical practices can take to successfully adopt these emerging technologies.
- The Growing Need for AI in Diagnostic Accuracy
- How AI Processes 15,000+ Data Points to Spot Hidden Disease Patterns
- Early Disease Detection: AI Identifies Diseases Before Symptoms Appear
- Medical Imaging AI: Enhancing Diagnostic Precision
- Challenges and Ethical Considerations in AI Healthcare Consulting
- AI-Powered Diagnostics: Transforming Healthcare Delivery and Patient Outcomes
The Growing Need for AI in Diagnostic Accuracy
Medical Diagnosis: The Hidden Challenges Behind Critical Health Decisions
Diagnostic accuracy faces significant challenges across healthcare.
Complex symptoms, overlapping conditions, and subtle disease presentations make perfect diagnosis an elusive goal.
Why is medical diagnosis so challenging?
Multiple factors complicate this critical process:
- Diseases present differently across patient populations
- Symptoms overlap between common and rare conditions
- Medical knowledge expands at an unprecedented rate
- Time constraints limit comprehensive data analysis
- Subtle patterns may appear only across years of patient data
In a 2022 report, researchers found that diagnostic error-related deaths represented approximately 25% of all medical error deaths, or an estimated 64,000 preventable deaths annually in the United States due to diagnostic error alone.
This sobering statistic highlights the critical need for improved diagnostic processes.
How AI Enhances Diagnostic Capabilities
AI systems complement clinical expertise by addressing specific diagnostic challenges.
These tools search millions of research papers in milliseconds, compare patient data against every documented disease pattern, identify subtle trends in lab values across years, maintain consistent analysis quality regardless of time or workload, and consider both common and rare conditions with equal attention.
These systems are also capable of detecting patterns that might otherwise go unnoticed. While physicians observe physical symptoms during examinations, AI systems are able to process thousands of data points, revealing subtle pattern combinations that signal specific diseases.
CHIEF: Harvard’s AI Breakthrough Achieves 94% Cancer Detection Accuracy
AI systems are demonstrating remarkable results in real-world clinical settings, with documented improvements in both diagnostic accuracy and early disease detection.
Harvard Medical School researchers recently developed CHIEF (Clinical Histopathology Imaging Evaluation Foundation), a versatile AI model that operates like ChatGPT but specializes in cancer evaluation.
This system analyzes digital slides of tumor tissues with nearly 94% accuracy in cancer detection, outperforming current AI approaches across 11 cancer types. On previously unseen slides from surgically removed tumors, CHIEF maintained over 90% accuracy across multiple cancer types including colon, lung, breast, endometrium, and cervix.
Beyond simple detection, CHIEF predicts tumor genetic profiles without requiring expensive and time-consuming DNA sequencing. This capability is particularly valuable in identifying genomic variations that influence treatment response, with accuracy rates exceeding 70% for 54 commonly mutated cancer genes.
For specific treatment-related mutations, CHIEF’s accuracy reaches as high as 96% for EZH2 mutations in diffuse large B-cell lymphoma.
These advancements in diagnostic AI have significant implications for clinical decision-making and have the potential to transform how healthcare providers approach patient care through enhanced diagnostic capabilities and personalized treatment planning.
AI-Enhanced Diagnostics: How AI Processes 15,000+ Data Points to Spot Hidden Disease Patterns
The Data Overwhelm in Modern Medicine
Modern medicine generates an overwhelming amount of patient data.
Consider a single complex case: a 58-year-old woman presents with fatigue, joint pain, and mild fever. Her electronic health record contains:
- 15 years of lab results
- 8 specialist consultation notes
- 6 imaging studies
- 2 genetic test panels
- 47 medication records
- Thousands of documented vital signs
Each data point might contain critical diagnostic clues. Traditional diagnostic approaches might focus on recent symptoms and tests, potentially missing patterns visible only when analyzing the complete dataset.
Modern medical AI addresses this data complexity by performing multiple sophisticated analyses simultaneously. These systems process thousands of patient notes through Natural Language Processing, map genetic markers to potential conditions, connect seemingly unrelated symptoms through pattern recognition, identify relevant findings across years of medical records, and compare patient profiles to millions of similar cases.
Their computational power allows them to identify subtle correlations that might be missed in traditional clinical reviews due to time constraints or the natural limitations of human pattern recognition.
Moreover, these AI systems continue learning as they analyze new data, constantly refining their diagnostic capabilities based on outcomes and treatment responses. While AI systems build knowledge from vast clinical datasets, they continuously analyze patterns across populations while applying insights to individual patients.
AI in Specialized Medicine: SLIViT: UCLA’s Self-Learning AI Masters 3D Medical Imaging with Minimal Training Data
UCLA researchers have developed a breakthrough AI diagnostic system that’s transforming how specialists interpret complex medical imaging. Their deep-learning framework, called SLIViT (SLice Integration by Vision Transformer), teaches itself to analyze volumetric medical scans with accuracy matching medical specialists but completes the task thousands of times faster.
Unlike traditional AI models limited to specific imaging types or body systems, SLIViT demonstrates remarkable versatility across multiple imaging modalities. The system has been successfully tested with 3D retinal scans for disease biomarkers, ultrasound videos for heart function assessment, 3D MRI scans for liver disease severity, and 3D CT for chest nodule malignancy screening.
“What thrilled me most was SLIViT’s remarkable performance under real-life conditions, particularly with low-number training datasets,” explains Dr. SriniVas R. Sadda, professor of Ophthalmology at UCLA Health and Artificial Intelligence & Imaging Research director at the Doheny Eye Institute. “SLIViT thrives with just hundreds – not thousands – of training samples for some tasks, giving it a substantial advantage over other standard 3D-based methods in almost every practical case related to 3D biomedical imaging annotation.”
This efficiency breakthrough addresses a critical bottleneck in clinical AI implementation. While volumetric (3D) images provide valuable diagnostic information, they require significantly more time and expertise to interpret than standard 2D images.
For example, a single 3D retinal scan may comprise nearly 100 individual 2D images, requiring several minutes of close inspection by a highly trained specialist to detect subtle disease biomarkers or measure anatomical changes.
SLIViT overcomes these challenges by leveraging what researchers call “medical knowledge” from more accessible 2D imaging domains, allowing it to achieve superior performance with modest training datasets. This capability dramatically expedites the annotation process for non-annotated volumes while maintaining specialist-level accuracy.
“When a new disease-related risk factor is identified, it can take months to train specialists to accurately annotate the new factor at scale in biomedical images,” notes Dr. Eran Halperin, professor at UCLA’s Computational Medicine Department. “But with a relatively small dataset, which a single trained clinician can annotate in just a few days, SLIViT can dramatically expedite the annotation process for many other non-annotated volumes, achieving performance levels comparable to clinical specialists.”
The system’s potential benefits extend beyond efficiency gains.
By improving diagnostic timeliness and reducing the burden on clinical specialists, SLIViT promises to enhance patient care while simultaneously advancing medical research through reduced data acquisition costs and accelerated development of future predictive models.
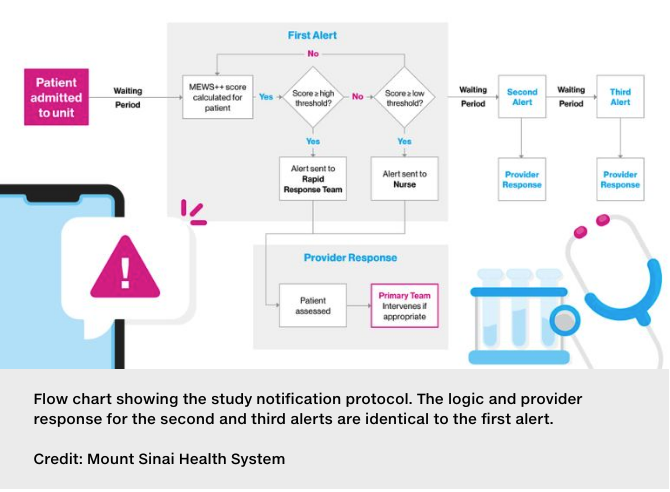
Measurable Improvements: Mount Sinai’s AI System Saves Lives Through Early Detection with 43% Higher Intervention Rate
Mount Sinai Hospital has documented significant outcomes after implementing their AI-driven clinical decision support system.
A non-randomized, prospective study examining 2,740 adult patients found that those whose care teams received real-time AI-generated alerts about potential health deterioration were 43 percent more likely to have their care escalated compared to patients whose alerts were created but not sent to providers.
This improved intervention timing translated to measurable clinical benefits. Patients in the intervention group receiving AI-generated alerts were:
- More likely to receive medications supporting heart and circulation, indicating earlier clinical action
- Significantly less likely to die during hospitalization
- Less likely to die within 30 days after admission
Dr. David L. Reich, President of The Mount Sinai Hospital, describes these tools as “augmented intelligence” that speeds up in-person clinical evaluations by physicians and nurses, prompting treatments that keep patients safer. The system helps “bring the right team to the right patient at the right time,” functioning as an accurate and timely aid to clinical decision-making.
Following successful initial testing, Mount Sinai has expanded the AI system to all stepdown units within the hospital using a simplified workflow, with intensive care physicians visiting the 15 highest-risk patients daily and making treatment recommendations to the primary care team.
This integrated approach allows the algorithm to continuously improve through reinforcement learning as it processes more patient data. The institution has since developed and deployed 15 additional AI-based clinical decision support tools throughout their health system, demonstrating how AI augments clinical expertise by analyzing patterns and identifying at-risk patients before traditional methods would detect decline.
Early Disease Detection: AI Identifies Diseases Before Symptoms Appear
Survival Disparities Reveal the Critical Time Window
Early disease detection fundamentally changes treatment outcomes.
Consider the stark statistics:
- Breast cancer: 98% five-year survival at stage I vs. 30% at stage IV
- Colon cancer: 91% survival when caught early vs. 10-15% in late stages
- Alzheimer’s: Treatments slow progression by 27% when started pre-symptomatically
- Heart disease: Preventive interventions can reduce the risk of heart disease by 80% when identified early
- Diabetic kidney disease: Early intervention can decrease the risk of renal impairment by 50%.
Traditional diagnostic approaches face inherent limitations.
Most reliably detect disease only after symptoms appear, when conditions have already progressed and treatments prove less effective.
This creates a critical diagnostic gap between disease onset and clinical manifestation.
Advancing Detection Capabilities Through AI
Google has developed an AI system for mammography that matches radiologist accuracy in breast cancer detection. The system analyzes thousands of de-identified mammograms to identify subtle cancer indicators that even specialists might miss.
With over 2 million breast cancer diagnoses annually, this technology addresses global screening bottlenecks by prioritizing high-risk cases and reducing diagnostic delays. Current research partnerships with Northwestern Medicine, Imperial College London, and NHS trusts are evaluating the AI as a “second independent reader” in clinical settings.
The system shows particular promise for improving screening consistency while allowing radiologists to focus on complex cases. As Professor Yusuke Nakamura notes, “By using AI technology for cancer screening, we can maintain the accuracy of diagnosis and reduce the burden on radiologists, even if many people undergo medical checkup.”
These advancements extend beyond imaging:
- Voice analysis algorithms developed by researchers can detect Parkinson’s disease through subtle speech changes. These AI models identify minute variations in pitch, articulation, and rhythm caused by diminished control over vocal muscles—achieving up to 99% accuracy in some studies. Associate Professor Ali Al-Naji explains: “Vocal changes are early indicators of Parkinson’s disease… By analyzing these acoustic features, AI models can detect subtle, disease-related vocal patterns long before visible symptoms appear.”
- Stanford’s retinal scanning AI identifies clinical biomarkers to predict early-onset Alzheimer’s Disease and mild cognitive impairment.
- Johns Hopkins’ blood test AI recognizes pancreatic cancer signatures from routine lab results.
Each system identifies subtle disease signatures that emerge long before clinically apparent symptoms, addressing fundamental limitations in traditional screening approaches.
Beyond detection, these technologies offer remote monitoring capabilities, reducing the need for in-person visits while maintaining high standards of care.
Researchers continue working to ensure these technologies work effectively across diverse populations, both improving detection rates and potentially reducing healthcare disparities in early disease identification.
AI Uncovers Disease Fingerprints Human Doctors Cannot See: Finding Signals in Sparse Data
AI doesn’t just improve existing diagnostic methods—it finds entirely new ways to detect disease early. For rare diseases affecting over 350 million people worldwide, AI can identify previously unknown patterns that signal disease before symptoms appear.
Recent research shows AI systems can discover new biomarkers even with limited data. In one study of a rare bone condition caused by neurofibromatosis, algorithms identified specific markers like cartilage formation rate that predict treatment success. Support Vector Machine and Random Forest algorithms work effectively despite the small datasets typically available for rare conditions.
Bayesian network approaches offer another solution, grouping disease subtypes and identifying relationships between conditions. These systems create patient clusters that reveal important patterns doctors might otherwise miss.
By finding these early disease indicators, AI creates opportunities for treatment when it’s most effective, potentially changing the course of diseases that were previously difficult to diagnose and treat.
Medical Imaging AI: Enhancing Diagnostic Precision
The Impossibility of Perfect Human Analysis
Medical imaging presents unique diagnostic challenges. A single chest CT contains hundreds of slices with millions of pixels. A subtle 3mm lung nodule might occupy just a few pixels within this vast dataset.
Similar challenges exist across all imaging modalities:
- Microscopic abnormalities in dense breast tissue on mammography
- Hairline fractures barely visible on emergency X-rays
- Early ischemic changes on stroke CT visible only through subtle density differences
- Small metastases hidden among normal anatomical structures on abdominal CT
- Early retinal changes indicating systemic disease
These detection challenges are compounded by increasing imaging volumes. Radiologists at busy hospitals may interpret a new study every 3-4 minutes during peak periods. Meanwhile, image resolution continues to increase, with each study containing more data requiring analysis.
AI transforms these challenges into opportunities by:
- Detecting minute abnormalities through pixel-level analysis
- Quantifying tumor characteristics with millimeter precision
- Identifying subtle fractures through bone density pattern recognition
- Comparing current images with prior studies to highlight changes
- Standardizing measurements across different imaging studies
Stanford University’s CheXNet exemplifies these capabilities. CheXNet simultaneously evaluates X-rays for 14 different pathologies in about 90 seconds, while radiologists required three hours on average to review the same images. The system achieved radiologist-level performance on 11 of 14 conditions, including masses, enlarged hearts, and collapsed lungs.
“Usually, we see AI algorithms that can detect a brain hemorrhage or a wrist fracture – a very narrow scope for single-use cases,” explained Dr. Matthew Lungren, assistant professor of radiology at Stanford. “But here we’re talking about 14 different pathologies analyzed simultaneously, and it’s all through one algorithm.”
From Slides to Cellular Maps: AI Transforms Pathology Diagnosis
Pathology diagnosis presents similar challenges including analyzing complex biological samples across multiple stains and magnifications. Traditional microscopic analysis requires hours of careful examination to find and characterize abnormal cells among millions of normal ones.
AI pathology systems can address these challenges by:
- Scanning whole slides at cellular resolution in minutes
- Identifying abnormal cells with consistent accuracy
- Classifying cancer subtypes through pattern recognition
- Quantifying biomarker expression objectively
- Predicting disease progression from cellular characteristics
These capabilities dramatically transform pathology workflows and diagnostic accuracy. Pathologists using AI can complete cases faster with improved accuracy compared to traditional approaches. For patients awaiting cancer diagnosis, this can mean receiving same-day results instead of waiting multiple days.
The integration of AI into pathology also enables more sophisticated analysis. By examining subtle cellular features invisible to the human eye, these systems can identify specific genetic mutations and predict treatment responses before therapy begins. This level of precision helps guide treatment decisions, particularly for complex cases where traditional analysis might miss important prognostic indicators.
As with other medical imaging applications, AI pathology tools don’t replace human expertise but rather enhance it by handling the most labor-intensive aspects of tissue analysis.
This partnership between AI and pathologists represents another important advance in how technology is transforming diagnostic medicine across specialties.
Challenges and Ethical Considerations in AI Healthcare Consulting
Patient Data Protection: Balancing Innovation with HIPAA and GDPR Compliance
Healthcare AI systems require access to sensitive patient information, creating complex data protection challenges. Successful AI integration must address several key privacy considerations:
- Protecting patient data throughout AI processing pipelines
- Securing data transfers between clinical and AI systems
- Implementing appropriate access controls and authentication
- Maintaining compliance across cloud and on-premise components
- Providing transparency to patients about data utilization
Healthcare AI consultants help organizations navigate complex regulatory frameworks including HIPAA, GDPR, and state-specific privacy laws. Privacy breaches result in significant penalties, damaged institutional trust, and potential harm to patients. By addressing these challenges proactively, organizations can implement AI solutions while maintaining patient confidentiality.
Hidden Healthcare Disparities: How Biased Algorithms Amplify Inequity in Patient Care
AI algorithms used in healthcare inevitably reflect the data they’re trained on, which can perpetuate existing healthcare disparities if left unchecked. These biases emerge throughout the AI development lifecycle from data collection through model implementation, and can significantly impact clinical decision-making.
Imbalanced representation in training data remains a fundamental challenge. Many medical datasets overrepresent certain demographic groups, leading to algorithms that perform worse for underrepresented populations. This performance gap isn’t merely technical; it directly affects who benefits from AI-driven healthcare improvements.
Missing or incomplete data creates additional bias risks. Patients with lower socioeconomic status often have more fragmented medical records across multiple healthcare systems, leading AI systems to systematically underestimate their risks or miss important clinical factors. Similarly, social determinants of health such as access to care, social support networks, and housing significantly impact patient outcomes but are rarely captured comprehensively in medical records.
Even the labels used to train AI models can introduce bias. When algorithms learn from diagnoses made by human clinicians, they may perpetuate implicit cognitive biases related to gender, race, or other patient attributes. These biases can affect everything from diagnosis accuracy to treatment recommendations.
Effective bias mitigation requires multifaceted approaches. During development, subgroup analysis should evaluate model performance across different patient populations. Model interpretability techniques can reveal how an algorithm’s decision-making might differ across demographic groups. Statistical debiasing methods can adjust for underrepresented groups without sacrificing overall performance.
Most critically, AI systems require rigorous validation before clinical implementation. Ongoing monitoring should detect bias in real-world settings, with feedback mechanisms to capture why and when clinicians might override AI recommendations for certain patient groups. Through these comprehensive approaches, healthcare organizations can harness AI’s benefits while working to ensure all patients benefit equitably from these technological advances.
Beyond Implementation: Creating a Physician-Centered AI Ecosystem
Successful healthcare AI implementation requires thoughtful integration into existing clinical workflows rather than imposing technology for its own sake. As Dr. Stephen Parodi of The Permanente Medical Group explains, “This is not just an IT thing… this is about how we actually practice.”
Organizations implementing AI must establish appropriate governance structures involving physicians, hospital leadership, and health plan partners in active dialogue about what’s being implemented and how it’s performing. This multidisciplinary approach should include bioethicists to address the ethical considerations alongside operational ones.
Transparency with both physicians and patients is essential when implementing AI tools. All stakeholders should be aware of how the technology is being used and for what purposes. Permanente Medical Group has already demonstrated measurable benefits from AI implementation, including mortality benefits in hospital settings and reductions in emergency visits when used in ambulatory care.
To ensure AI enhances rather than disrupts care, leaders must frame AI as a tool that augments clinical practice—not as a replacement for clinical judgment. This perspective has allowed Permanente to achieve significant workflow improvements, such as reducing documentation time by one to two hours per day for clinicians using ambient AI for note generation.
However, successful implementation also requires ongoing monitoring systems to ensure AI tools don’t introduce unintended biases or inequities in care delivery. As Dr. Parodi notes, “We want to make sure that we don’t introduce unintended biases into our practice because of predisposing assumptions that are in an electronic health record that AI is scraping.”
The organizations that successfully implement AI will be those that develop clear metrics for success, involve physicians at all levels of leadership, and remain vigilant about equity considerations while recognizing that regulation is inevitable. With physician involvement in setting “the rules of the road,” AI can fulfill its promise as a tool that genuinely improves care rather than complicating it.
AI-Powered Diagnostics: Transforming Healthcare Delivery and Patient Outcomes
AI transforms healthcare by processing vast amounts of medical data beyond human capacity. It detects diseases earlier and analyzes complex information with consistency that humans cannot match. Hospitals using these systems find cancers sooner and diagnose heart conditions and rare diseases faster. These improvements directly enhance patient outcomes. Earlier disease detection expands treatment options and increases intervention effectiveness, potentially reducing healthcare costs and extending patient lives.
AI also changes how providers work daily in meaningful ways. Doctors spend less time reviewing thousands of data points because AI highlights what needs attention. Systems complete in minutes what would take humans hours which frees up physicians to see more patients or focus on complex cases. AI offers a reliable second opinion for difficult diagnoses while ambient systems cut documentation time by hours each day. This shift allows providers to focus on what matters most – connecting with patients and solving complex medical problems.
That being said, successful implementation requires strategic expertise. Healthcare AI consulting provides this essential expertise, ensuring new systems complement clinical practice, address specific challenges, and maintain regulatory compliance, while delivering measurable improvements without disrupting established workflows.
Healthcare organizations that adopt AI strategically gain significant advantages in diagnostic capabilities while improving providers’ ability to deliver better and more focused care. Thus, healthcare organizations must choose: invest strategically in AI tools with expert guidance or risk falling behind.