Should healthcare apps fostering value-based care and pay-per-visit models differ at all? It’s a question that might seem straightforward but opens up a world of strategic considerations. Both models fundamentally focus on patient care, yet they operate on different principles and may require distinct features to cater to their unique demands.
Value-based care emphasizes patient outcomes, rewarding providers for quality care and preventative measures. In contrast, pay-per-visit care ensures providers are compensated for each service, simplifying billing but potentially overlooking long-term health benefits. So, can a single app seamlessly integrate both models, or is it more practical to prioritize one over the other?
At Topflight, we believe in exploring these nuanced questions to deliver solutions that truly meet the needs of modern healthcare. By examining whether a hybrid approach is viable—or if focusing on a single model is more beneficial for your organization—we aim to provide insights that guide effective decision-making and app development.
Ready to delve deeper into this critical discussion? Let’s explore the complexities and opportunities of creating a medical app that bridges the gap between value-based care and pay-per-visit models, ensuring optimal patient care and operational efficiency.
Top Takeaways:
- Hybrid Model Integration for Comprehensive Care: Developing a medical app that supports both Value-Based Care (VBC) and Pay-Per-Visit (PPV) models allows for a balanced approach to healthcare. VBC focuses on patient outcomes, preventative care, and quality, incentivizing providers based on performance and health results. PPV, on the other hand, offers straightforward billing and operational simplicity. By integrating these models, a healthcare app can cater to diverse patient needs and preferences, ensuring both high-quality care and financial sustainability. This hybrid approach can also enhance patient engagement and satisfaction by offering flexible care options.
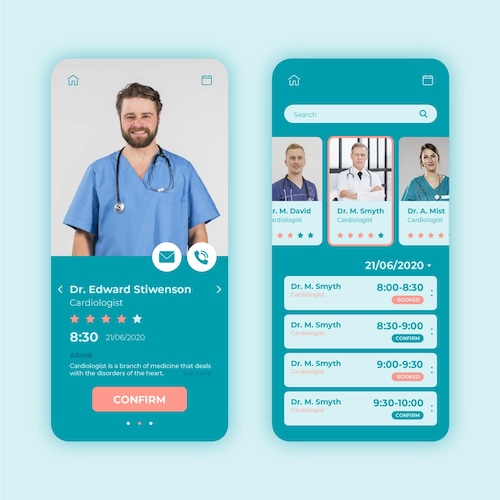
- Core Features and User-Centered Design: To create a viable medical app, focus on core features that support both VBC and PPV models. These include patient management and engagement tools (appointment scheduling, telehealth), data analytics and reporting for VBC, and billing and payment processing for PPV. Additionally, seamless interoperability with EMRs and HIPAA compliance are essential for continuity of care. A user-centered design approach is critical, ensuring the app is intuitive, accessible, and meets the needs of diverse user groups, including patients and providers.
Table of Contents:
- Deciphering the Synergies Between Value-Based and Pay-Per-Visit Healthcare Models
- Market Analysis and Needs Assessment
- Regulatory and Compliance Considerations
- Core Features of a Viable Medical App
- Design and User Experience
- Technology Stack and Development Considerations
- Data Management and Analytics
- Implementation and Deployment
- Challenges and Solutions
- Topflight’s Expertise in Hybrid Healthcare Apps
Deciphering the Synergies Between Value-Based and Pay-Per-Visit Healthcare Models
To create a healthcare app that effectively integrates both Value-Based Care and Pay-Per-Visit care models, it’s essential to understand the fundamentals of each approach and how they can work together in a hybrid system.
Value-Based Care Model
Value-Based Care is a transformative approach in healthcare that prioritizes patient outcomes and the overall quality of care rather than the volume of services provided. The essence of VBC lies in its focus on preventative care, chronic disease management, and the continuous improvement of health outcomes. Providers under VBC are incentivized to deliver high-quality care through various performance metrics such as patient satisfaction scores, readmission rates, and overall health improvements.
Key components of VBC include:
- Patient-Centered Approach: Care plans are tailored to individual patient needs, promoting better engagement and adherence to treatment.
- Preventative Measures: Emphasis on early detection and prevention of diseases to reduce long-term healthcare costs.
- Outcome-Based Incentives: Providers are rewarded based on the effectiveness and efficiency of the care they provide, encouraging continual improvement in healthcare delivery.
Pay-Per-Visit Care Model
Pay-Per-Visit care, also known as fee-for-service, is a traditional healthcare model where providers are compensated based on the number of services they deliver. Each consultation, procedure, or treatment is billed separately, creating a straightforward and easily understandable billing system for both providers and patients.
Key features of PPV include:
- Service-Based Billing: Providers charge for each individual service rendered, simplifying the billing process.
- Operational Simplicity: The clear and direct nature of PPV makes it easy to implement and manage from an administrative perspective.
- Financial Predictability: Providers receive predictable revenue streams based on the volume of services provided.
Key Differences and Synergies
While VBC and PPV represent different financial incentives and operational philosophies, they can complement each other when thoughtfully integrated into a hybrid model. Here’s how:
Differences:
- Financial Incentives: VBC focuses on quality and outcomes, while PPV is driven by service quantity.
- Care Approach: VBC emphasizes comprehensive, ongoing care, whereas PPV often focuses on episodic, immediate treatment.
- Patient Interaction: VBC encourages long-term patient relationships and engagement, while PPV interactions can be more transactional.
Synergies:
- Comprehensive Care: By combining the strengths of both models, healthcare providers can offer a more robust and flexible care delivery system. The preventative and outcome-focused nature of VBC can enhance the efficiency and effectiveness typically associated with PPV.
- Balanced Incentives: A hybrid approach ensures that providers are motivated to deliver high-quality care while also being compensated for the volume of necessary services.
- Enhanced Patient Experience: Patients benefit from the comprehensive, proactive care of VBC, alongside the accessibility and simplicity of PPV services.
By understanding and leveraging the unique strengths of both VBC and PPV, healthcare app developers can create solutions that cater to diverse patient needs and provider capabilities. This balanced approach not only improves patient outcomes but also enhances the operational efficiency and financial sustainability of healthcare practices.
Market Analysis and Needs Assessment
Creating a viable medical app that serves both VBC and Pay-Per-Visit models requires an in-depth understanding of the market demands, patient needs, and provider requirements. This section delves into these critical aspects to ensure your healthcare application is both relevant and effective.
Identifying Market Demands
The healthcare industry is rapidly evolving, with digital health solutions becoming increasingly integral to patient care. Understanding these trends is vital for developing a successful hybrid app:
- Telemedicine Growth: The COVID-19 pandemic accelerated the adoption of telemedicine, with many patients and providers continuing to prefer virtual appointments for their convenience. In 2021, 37% of U.S. adults used telemedicine, with more females (42%) than males (31.7%) engaging in virtual care. By 2024, over 116 million users worldwide had participated in online doctor consultations, a substantial increase from around 57 million in 2019. Telemedicine continues to thrive due to its convenience and efficiency, with 87% of patients expressing satisfaction with their telemedicine experiences.
- Data-Driven Decision Making: Healthcare organizations are leveraging big data and analytics to enhance patient outcomes and operational efficiency. Integrating data from consumer devices into patient records provides a comprehensive view of patient health, facilitating better decision-making and personalized care.
- Patient-Centric Solutions: Modern patients expect personalized care experiences facilitated by digital tools that offer convenience and transparency.
By targeting these market demands, your app can address current gaps and position itself as a valuable tool in the evolving healthcare landscape.
Analyzing Patient Needs and Preferences
Understanding patient behavior and preferences is crucial for designing an app that truly engages users and meets their expectations. Key considerations include:
- Ease of Use: A user-friendly interface is essential. Patients should be able to navigate the app intuitively, whether they’re scheduling appointments, accessing medical records, or communicating with providers.
- Engagement Tools: Features like appointment reminders, medication tracking, and lifestyle tips can help keep patients engaged and proactive about their health.
- Personalization: Patients appreciate tailored content and recommendations based on their medical history and current health status, enhancing the overall care experience.
Patients today are tech-savvy and expect seamless, responsive digital interactions. Ensuring your app meets these expectations is key to its success.
Assessing Provider Requirements
For healthcare providers, a hybrid app must integrate seamlessly into their existing workflows and comply with clinical protocols. Important factors to consider include:
- Workflow Integration: The app should support and enhance existing workflows, not disrupt them. This includes integration with Electronic Medical Records (EMRs) and other clinical systems.
- Ease of Use for Providers: Just as ease of use is important for patients, it’s equally critical for providers. The app should streamline administrative tasks and help providers manage patient care more efficiently.
- Compliance and Reporting: Ensure that the app complies with healthcare regulations like HIPAA and GDPR. It should also facilitate easy reporting and documentation to support both VBC and PPV models.
Providers need tools that enhance their ability to deliver high-quality care while simplifying administrative burdens. Addressing these requirements will make your app an invaluable asset to healthcare practices.
Regulatory and Compliance Considerations
Ensuring your healthcare app is compliant with regulations is crucial to its success and credibility. Non-compliance can lead to severe penalties and loss of trust among users. Here’s how to navigate the maze of healthcare regulations effectively.\
Compliance Requirements for VBC and PPV Models
Different care models are still bound by the same HIPAA compliance requirements. Here’s how to ensure your app meets those requirements:
- Value-Based Care Compliance: VBC emphasizes patient outcomes and involves sharing data across various healthcare providers and payers. Ensuring that all shared data is secure and compliant with relevant regulations is critical. Compliance requirements include data encryption, secure data transmission, and comprehensive audit trails.
- Pay-Per-Visit (PPV) Compliance: PPV involves straightforward billing and operational simplicity, but it still requires adherence to billing standards and patient consent protocols. Ensuring accurate billing practices, maintaining detailed records, and safeguarding patient consent forms are fundamental.
Ensuring Data Security and Patient Privacy
Data security and patient privacy are paramount when developing a healthcare app. Here are best practices to maintain robust security and privacy:
- Data Encryption: Ensure all patient data is encrypted both at rest and in transit. This prevents unauthorized access and ensures that even if data is intercepted, it remains unreadable.
- Access Controls: Implement strict access controls to ensure that only authorized personnel can access sensitive data. Role-based access control can help limit data exposure to necessary personnel only.
- Regular Audits and Monitoring: Conduct regular security audits and continuously monitor your systems for potential vulnerabilities. Promptly address any identified gaps to prevent breaches.
- Patient Consent: Clearly communicate how patient data will be used and obtain explicit consent before collecting any data. Ensure that patients have the option to withdraw their consent at any time.
- Compliance Documentation: Maintain comprehensive documentation of your compliance efforts, including policies, procedures, and audit logs. This documentation can be invaluable during regulatory reviews and audits.
By adhering to these regulatory and compliance guidelines, you can build a healthcare app that not only meets legal requirements but also earns the trust of users.
Core Features of a Viable Medical App
Creating a medical app that effectively serves both Value-Based Care and Pay-Per-Visit models requires incorporating a comprehensive set of features designed to enhance patient outcomes, streamline operations, and ensure compliance. Here’s an in-depth look at the core features your app should include:
Patient Management and Engagement Tools
Engaging patients and managing their interactions efficiently is fundamental to the success of any healthcare app. Key tools include:
- Appointment Scheduling: Allow patients to book, reschedule, and cancel appointments easily. Integration with provider calendars ensures availability is up-to-date.
- Reminders and Notifications: Automated reminders for appointments, medication adherence, and health tips can significantly reduce no-show rates and improve patient engagement.
- Telehealth Capabilities: Support for video consultations and asynchronous communication enables providers to offer care remotely, enhancing convenience for patients.
- Patient Education Resources: Provide access to educational materials, tutorials, and FAQs to help patients better understand their conditions and treatments.
These tools not only enhance patient satisfaction but also contribute to more efficient practice management.
Data Analytics and Reporting for Value-Based Care
In the VBC model, data analytics play a crucial role in improving patient outcomes and operational efficiency. Important features include:
- Real-Time Data Collection: Continuously gather data from various sources, including wearable devices, to provide a holistic view of patient health.
- Advanced Analytics: Utilize machine learning and AI to analyze data trends, predict patient outcomes, and identify high-risk patients.
- Customizable Reporting: Enable providers to generate detailed reports on patient outcomes, performance metrics, and compliance with VBC protocols.
- Outcome Measurement: Track key performance indicators (KPIs) such as readmission rates, patient satisfaction scores, and treatment adherence to evaluate the effectiveness of care provided.
Effective use of data analytics helps providers make informed decisions, enhancing both patient care and operational efficiency.
Billing and Payment Processing for PPV
To support the PPV model, your app must have robust billing and payment processing features. These should include:
- Streamlined Billing: Automate the billing process to ensure accuracy and efficiency. This includes generating invoices, processing payments, and managing claims.
- Multiple Payment Options: Offer patients various payment methods, including credit/debit cards, digital wallets, and installment plans.
- Transparent Pricing: Clearly display costs for services to avoid surprises and build trust with patients.
- Financial Reporting: Provide detailed financial reports to help providers track revenue, outstanding payments, and financial performance.
A seamless billing system improves revenue cycle management and enhances the patient experience by simplifying the payment process.
Read more on healthcare payment system integration
Interoperability and Integration with EMRs
Interoperability is essential for ensuring continuity of care and efficient workflow integration. Key considerations include:
- Seamless EMR Integration: Ensure the app can integrate with existing Electronic Medical Records (EMRs) to provide a unified view of patient data across different systems.
- Data Exchange Standards: Adhere to standards like HL7 and FHIR to facilitate smooth data exchange between the app and other healthcare systems.
- API Support: Develop robust APIs to enable easy integration with third-party applications, such as lab systems, pharmacies, and insurance providers.
- Secure Data Sharing: Implement strict data security measures to ensure that shared data complies with regulations and maintains patient confidentiality.
By ensuring interoperability, you enable providers to deliver coordinated, efficient care that spans multiple healthcare settings.
Design and User Experience
Creating a successful healthcare app goes beyond just functional capabilities; it also requires an exceptional design and user experience (UX). A well-designed app not only improves patient engagement but also enhances provider efficiency. Here’s how to ensure your app excels in design and UX.
Importance of User-Centered Design
User-centered design (UCD) is a crucial approach that places the needs and expectations of users at the forefront. Here’s why it matters:
- Enhanced Usability: By focusing on the end-users—both patients and providers—you create an app that is intuitive and easy to navigate, reducing the learning curve.
- Increased Engagement: An app designed with users in mind encourages more frequent use, leading to better health outcomes and more efficient workflows.
- Higher Satisfaction Rates: Meeting user needs leads to higher satisfaction rates and positive feedback, which is essential for the app’s success and adoption.
Adopting UCD ensures that every design decision is made with the user in mind, resulting in a more effective and enjoyable experience.
Creating an Intuitive User Interface
An intuitive user interface (UI) is vital for minimizing user friction and enhancing the overall experience. Here are some guidelines:
- Simplified Navigation: Ensure that the app’s navigation is straightforward, with clear labels and logical pathways. Users should always know where they are and how to get to where they want to be.
- Consistent Design Elements: Use consistent design elements, such as buttons, icons, and fonts, to create a cohesive experience and reduce cognitive load.
- Responsive Design: Design the app to be responsive, ensuring it works seamlessly across various devices and screen sizes, from smartphones to tablets.
- Minimalist Approach: Avoid clutter by focusing on essential features and functions. A minimalist design helps users focus on what’s important without distractions.
By following these guidelines, you can create a UI that feels natural and easy to use, even for those who may not be tech-savvy.
Ensuring Accessibility for Diverse User Groups
Accessibility is a critical aspect of UX design, especially in healthcare, where users may have varying levels of tech proficiency and physical abilities. Key considerations include:
- Compliance with Accessibility Standards: Ensure your app complies with accessibility standards like the Web Content Accessibility Guidelines (WCAG). This includes providing alternative text for images, ensuring sufficient color contrast, and enabling keyboard navigation.
- Support for Assistive Technologies: Make sure the app is compatible with assistive technologies such as screen readers, voice recognition software, and magnification tools.
- User Testing with Diverse Groups: Conduct usability testing with a diverse group of users, including those with disabilities, to identify and address potential accessibility issues early in the development process.
- Customizable Features: Allow users to customize their experience, such as adjusting text size, enabling dark mode, or setting high-contrast themes, to meet their specific needs.
Ensuring accessibility not only broadens your user base but also demonstrates a commitment to inclusivity and patient-centric care.
Design and user experience are foundational elements of a successful healthcare app. By prioritizing user-centered design, creating an intuitive user interface, and ensuring accessibility, you can develop an app that stands out in the market and delivers significant value to both patients and providers.
Technology Stack and Development Considerations
Building a medical app that is viable for both value-based care and pay-per-visit care requires thoughtful selection of the technology stack and meticulous planning of development considerations. Here’s how to navigate this crucial aspect to ensure scalability, security, and efficient development.
Choosing the Right Technology Stack
Selecting the appropriate technology stack is fundamental to your app’s performance, scalability, and long-term viability. Here are some key components to consider:
- Frontend Technologies: For a responsive and intuitive user interface, consider using frameworks like React Native or Flutter. These allow for cross-platform development, ensuring that your app works seamlessly on both iOS and Android devices.
- Backend Technologies: Opt for robust backend frameworks such as Node.js, Django, or Ruby on Rails. These frameworks offer excellent support for building scalable and efficient server-side applications.
- Database Management: Choose databases that can handle large volumes of data efficiently. Options like PostgreSQL for relational data and MongoDB for NoSQL data are popular choices in the healthcare sector due to their reliability and scalability.
- APIs and Integration Tools: Ensure that your app can integrate with various third-party services and systems, especially Electronic Medical Records (EMRs). RESTful APIs and GraphQL are effective tools for creating flexible and scalable APIs.
- Cloud Services: Leverage cloud platforms like AWS, Google Cloud, or Microsoft Azure for hosting, storage, and other infrastructure needs. These platforms offer scalable solutions that can grow with your app’s user base.
Choosing the right technology stack sets the foundation for a robust, secure, and scalable healthcare app.
Scalability and Performance Optimization
Scalability and performance are critical to the success of your healthcare app, especially as your user base grows. Here are strategies to ensure your app performs optimally:
- Load Balancing: Implement load balancing to distribute incoming network traffic across multiple servers, ensuring no single server becomes a bottleneck.
- Caching: Use caching mechanisms to store frequently accessed data temporarily. Tools like Redis or Memcached can significantly improve data retrieval times and reduce server load.
- Microservices Architecture: Consider adopting a microservices architecture, where the app is divided into smaller, independent services. This approach enhances scalability and allows for more flexible and efficient management of different app components.
- Monitoring and Analytics: Implement monitoring tools like New Relic, Datadog, or Prometheus to track app performance in real-time. These tools help identify and address potential issues before they impact users.
By focusing on scalability and performance optimization, you ensure that your app remains responsive and reliable, even under increased load.
Integration with Existing Healthcare Systems
Seamless integration with existing healthcare systems is essential for providing comprehensive and coordinated care. Here are some technical considerations:
- Interoperability Standards: Adhere to interoperability standards like HL7 and FHIR to facilitate smooth data exchange between your app and other healthcare systems.
- Secure Data Transfer: Ensure that all data transfers between your app and external systems are secure. Use encryption protocols like TLS/SSL to protect data in transit.
- API Management: Develop robust APIs that allow for easy integration with third-party systems, including EMRs, lab systems, and pharmacies. Implement API gateways to manage and secure API traffic.
- Data Mapping and Transformation: Use data mapping and transformation tools to ensure that data exchanged between systems is accurate and consistent, minimizing errors and enhancing data quality.
Integrating seamlessly with existing healthcare systems enables your app to provide a unified and comprehensive view of patient data, enhancing the overall care experience.
Data Management and Analytics
Data management and analytics are pivotal to the success of a medical app that serves both VBC and PPV models. Proper data handling not only enhances patient outcomes but also ensures smooth billing processes and regulatory compliance. Here’s how to effectively manage and leverage data in your healthcare app.
Collecting and Analyzing Patient Data
Collecting comprehensive and accurate patient data is fundamental to providing high-quality care. However, it must be done while ensuring compliance with regulations and maintaining data integrity. Here are some best practices:
- Comprehensive Data Collection: Gather data from various sources such as Electronic Medical Records (EMRs), wearable devices, and patient self-reports. This provides a holistic view of the patient’s health status.
- Data Accuracy: Implement validation checks at data entry points to ensure accuracy. Regular audits and cleaning processes can help maintain data quality.
- Compliance: Ensure all data collection methods comply with regulations like HIPAA and GDPR. This includes obtaining informed consent from patients and ensuring data protection measures are in place.
- Real-Time Analytics: Utilize real-time data analytics to monitor ongoing patient health. This enables timely interventions and better patient management.
By focusing on accurate and compliant data collection, you lay the groundwork for effective analysis and decision-making.
Using Data for Quality Improvement in VBC
Data analytics is vital for improving care quality under the VBC model. Here’s how you can leverage data for better outcomes:
- Predictive Analytics: Use machine learning algorithms to predict patient outcomes and identify high-risk patients. This allows for proactive interventions and personalized care plans.
- Performance Metrics: Track key performance indicators (KPIs) such as readmission rates, patient satisfaction scores, and treatment adherence. These metrics help evaluate the effectiveness of care and identify areas for improvement.
- Clinical Decision Support: Integrate clinical decision support systems (CDSS) that use data analytics to provide evidence-based recommendations to healthcare providers. This supports informed decision-making and enhances care quality.
- Continuous Monitoring: Implement continuous monitoring systems that use data to track patient progress and adjust care plans as needed. This ensures that care remains effective and responsive to patient needs.
Using data effectively in VBC helps in delivering targeted, efficient, and high-quality care, ultimately improving patient outcomes and satisfaction.
Ensuring Accurate Billing in PPV
Accurate billing is critical in the PPV model to ensure financial sustainability and patient trust. Here are strategies to ensure billing accuracy:
- Automated Billing Systems: Implement automated billing systems that reduce manual errors by generating invoices based on predefined rules and integrated data sources.
- Insurance Claims Management: Develop robust claims management features that streamline the submission, tracking, and resolution of insurance claims. This reduces delays and improves cash flow.
- Billing Audits: Conduct regular billing audits to identify and rectify discrepancies. This ensures that all services provided are accurately billed and paid for.
- Transparency: Provide transparent billing information to patients, including detailed breakdowns of charges. This builds trust and helps patients understand their healthcare costs.
Effective data management and analytics are crucial for the success of a medical app serving VBC and PPV models. By focusing on accurate data collection, leveraging analytics for quality improvement, and ensuring billing accuracy, you create an app that not only enhances patient care but also streamlines operational efficiency.
Implementation and Deployment
Implementing and deploying a medical app that seamlessly supports both value-based care and pay-per-visit models requires meticulous planning and execution.
Project Management Best Practices
Effective project management is crucial for the successful development of your healthcare app. Here are some best practices to guide the process:
- Agile Methodologies: Adopt agile methodologies such as Scrum or Kanban to enable iterative development and continuous improvement. This allows for flexibility and quick adjustments based on feedback.
- Stakeholder Collaboration: Engage all stakeholders—including clinicians, developers, patients, and administrators—early in the planning stages. Regularly gather their input to ensure the app meets everyone’s needs.
- Clear Requirements: Define clear and detailed requirements at the outset. Use user stories and personas to capture the needs of different user groups and ensure that these requirements are prioritized appropriately.
- Milestones and Deliverables: Set realistic milestones and deliverables to track progress and maintain focus. Regularly review these milestones to ensure the project stays on track.
Effective project management ensures that the development process is organized, transparent, and aligned with the goals of all stakeholders.
Testing and Quality Assurance
Thorough testing and quality assurance (QA) are critical to ensuring your app functions correctly and securely. Here’s how to implement a robust QA strategy:
- Functional Testing: Conduct functional testing to ensure all features work as intended. This includes unit tests, integration tests, and system tests.
- Performance Testing: Evaluate the app’s performance under various conditions. Load testing and stress testing help identify potential bottlenecks and ensure the app can handle peak usage.
- Security Testing: Given the sensitive nature of healthcare data, security testing is paramount. Perform vulnerability assessments and penetration testing to identify and mitigate security risks.
- User Acceptance Testing (UAT): Involve end-users in UAT to validate that the app meets their needs and expectations. Gather feedback and make necessary adjustments before the final release.
- Regression Testing: Implement regression testing to ensure new updates or changes do not negatively impact existing functionality.
A comprehensive testing strategy guarantees that your app is reliable, secure, and ready for deployment.
Strategies for a Smooth Rollout
Rolling out a healthcare app requires careful planning to ensure a seamless transition for users. Here are strategies to facilitate a smooth rollout:
- Pilot Testing: Start with a pilot phase to test the app in a real-world setting with a small group of users. This helps identify any last-minute issues and gather valuable feedback.
- User Training: Provide comprehensive training for all user groups. This includes clinicians, administrative staff, and patients. Use tutorials, webinars, and hands-on sessions to ensure users are comfortable with the app.
- Support Systems: Establish robust support systems to assist users during the initial launch and beyond. Offer multiple support channels such as online help centers, chat support, and dedicated help desks.
- Feedback Loops: Create mechanisms for continuous feedback to capture user experiences and areas for improvement. Regularly update the app based on this feedback to enhance usability and functionality.
- Marketing and Communication: Develop a marketing and communication plan to inform users about the app’s launch, features, and benefits. Use newsletters, social media, and in-app notifications to keep users informed and engaged.
By following these strategies, you can ensure a successful and smooth rollout, maximizing user adoption and satisfaction.
Challenges and Solutions
Developing a medical app that successfully accommodates both VBC and PPV models involves navigating a range of challenges. Understanding these potential hurdles and how to overcome them is crucial to the success of your project. Here, we delve into the common challenges and offer practical solutions and best practices.
Common Challenges in Developing Hybrid Apps
Regulatory Hurdles: Navigating the complex regulatory landscape is a significant challenge. Healthcare apps must comply with various regulations such as HIPAA in the US, GDPR in Europe, and others depending on the region. Each of these regulations has stringent requirements for data privacy, security, and patient consent.
Integration Issues: Seamless integration with existing healthcare systems, particularly Electronic Medical Records (EMRs), can be daunting. Different systems may use disparate data formats and standards, making interoperability a technical challenge.
User Adoption: Ensuring that both patients and healthcare providers adopt and use the app effectively can be challenging. Users may resist change or find the app difficult to navigate, leading to poor engagement and utilization rates.
Maintaining Data Security: Protecting sensitive patient data from breaches and cyber-attacks is paramount. Healthcare data is a prime target for cybercriminals, and failing to secure this data can lead to severe consequences, including legal penalties and loss of trust.
Solutions and Best Practices to Overcome Challenges
Regulatory Compliance:
- Engage Legal Experts: Work with legal experts who specialize in healthcare regulations to ensure your app complies with all relevant laws and standards.
- Implement Robust Privacy Policies: Develop and enforce comprehensive privacy policies that detail how patient data will be collected, used, and protected.
- Regular Audits: Conduct regular compliance audits to identify and rectify any potential issues promptly.
Seamless Integration:
- Adopt Interoperability Standards: Use established standards like HL7 and FHIR to facilitate data exchange between your app and other systems.
- Flexible APIs: Develop flexible APIs that can adapt to various data formats and protocols, making integration smoother.
- Collaborate with Providers: Work closely with healthcare providers during development to understand their systems and ensure compatibility.
Boosting User Adoption:
- User-Centered Design: Prioritize user-centered design principles to create an intuitive and easy-to-use interface. Conduct usability testing with real users to gather feedback and make necessary adjustments.
- Comprehensive Training: Provide comprehensive training and support for both patients and providers. Offer tutorials, webinars, and hands-on training sessions to build confidence and competence.
- Engagement Strategies: Implement strategies to boost user engagement, such as personalized notifications, reminders, and rewards for regular use.
Ensuring Data Security:
- Data Encryption: Encrypt all sensitive data, both at rest and in transit, to prevent unauthorized access.
- Access Controls: Implement strict access controls to ensure that only authorized personnel can access sensitive information. Use multi-factor authentication (MFA) for added security.
- Continuous Monitoring: Continuously monitor your systems for potential security threats. Use advanced security tools and services to detect and respond to incidents swiftly.
- Regular Updates: Keep all software components up to date with the latest security patches and updates to protect against known vulnerabilities.
Developing a hybrid medical app that supports both VBC and PPV models comes with its set of challenges. However, with careful planning, adherence to best practices, and a focus on user needs and regulatory compliance, these challenges can be effectively managed.
Topflight’s Expertise in Hybrid Healthcare Apps
At Topflight, we specialize in building medical applications that effectively bridge value-based care and pay-per-visit models. Our extensive experience in the healthcare domain enables us to deliver solutions that meet complex clinical requirements while improving efficiency and patient outcomes. Below, we showcase two of our impactful projects: RTHM and Dedica Health.
Real-Time Health Monitoring (RTHM) Case Study
Challenge: RTHM set out to create a digital health ecosystem centered around real-time monitoring for conditions like Long COVID and ME/CFS. The goal was to facilitate better research, diagnostics, and remote care amidst a shortage of qualified providers and rising treatment costs.
Solution: Topflight helped RTHM build a robust MVP using no-code and low-code tools, ensuring rapid development and flexibility. This included a mobile app for patients and an admin area for RTHM staff.
Major Achievements:
- Solid MVP: Successfully launched an MVP that gained traction with patients.
- Fast Pivoting: Utilized no-code/low-code infrastructure, allowing quick adjustments based on new research.
- Security Compliance: Ensured strong security measures in line with HIPAA guidelines.
- Intuitive Design: Delivered an engaging design with interactive charts and automated reminders.
- Integration with Wearables: Incorporated third-party services like Apple Health and Google Fit, ensuring comprehensive health data collection.
Dedica Health Case Study
Challenge: The Heart Medical Group aimed to enhance its cardiology practice with a remote patient monitoring (RPM) platform to increase efficiency and comply with Medicare guidelines. They needed to replace error-prone systems and reduce manual tasks.
Solution: Topflight developed an intuitive RPM platform that integrates with clinically certified medical sensors. This platform allowed doctors to monitor patients remotely, streamline back-office tasks, and maintain compliance with Medicare requirements.
Major Achievements:
- Daily Monitoring: Over 1,100 patients monitored daily through the platform.
- Revenue Growth: the client secured a $300,000 ARR deal via a SaaS subscription model for RPM services.
- Medicare Compliance: More than 80% of patients met CPT code targets, ensuring reimbursement.
- Back-Office Automation: Automated routine tasks, reducing administrative workload.
- Patient-Centric Design: Postponed mobile app development in favor of SMS communication to enhance patient engagement and compliance.
These case studies illustrate Topflight’s ability to deliver innovative, high-impact healthcare solutions that integrate VBC and PPV models. By focusing on user-centered design, seamless integration, and leveraging advanced technologies, we empower healthcare organizations to provide superior care while achieving operational efficiencies.
Are you ready to transform your healthcare delivery with a tailored app solution? Contact Topflight today to discuss how we can help you build a groundbreaking healthcare application.
For more information or to start your project with us, reach out at Topflight.
Frequently Asked Questions
Do healthcare apps need to cater to both value-based care and (VBC) and pay-per-visit (PPV) models, or can they focus on one?
Healthcare apps can be designed for either VBC or PPV, but a hybrid approach offers several advantages. Comprehensive Care: Combines preventative and ongoing care (VBC) with accessible, episodic care (PPV). Balanced Incentives: Providers are rewarded for quality care (VBC) while being compensated for necessary services (PPV). Enhanced Patient Experience: Offers patients flexibility and a wider range of care options.
What are the core features a VBC/PPV healthcare app should have?
A successful app needs features for both patients and providers. Patient Management & Engagement: Appointment scheduling, reminders, telehealth, educational resources. Data Analytics & Reporting (VBC): Real-time data collection, advanced analytics, customizable reports. Billing & Payment Processing (PPV): Streamlined billing, multiple payment options, transparent pricing. Interoperability & EMR Integration: Seamless integration with electronic medical records (EMRs).
How important is user experience (UX) design for a medical app?
UX design is crucial for both patient engagement and provider efficiency. Here’s why. User-Centered Design: Prioritizes user needs for an intuitive and easy-to-use app. Increased Engagement: A well-designed app encourages frequent use, leading to better health outcomes. Accessibility: Ensures the app caters to diverse users with varying tech skills and abilities.
What are some security considerations for developing a healthcare app?
Security is paramount when dealing with sensitive patient data. Here are key practices. Compliance with HIPAA and GDPR: Ensures data security and patient privacy. Data Encryption: Protects data at rest and in transit. Access Controls: Limits access to sensitive data based on user roles. Regular Audits & Monitoring: Identifies and addresses potential security vulnerabilities.
How can I ensure my app is successful in the long run?
Sustainability requires ongoing effort. Here are some key strategies. Data Management & Analytics: Leverage data to improve patient care, billing accuracy, and overall app functionality. Project Management: Use agile methodologies and clear communication to maintain focus and adapt to changing needs. Testing & Quality Assurance: Rigorous testing ensures a reliable, secure, and user-friendly app. Feedback Loops: Continuously gather user feedback to identify areas for improvement and keep the app relevant.