Cancer care doesn’t fail in the chemo chair; it fails in the quiet chaos in-between appointments—the lost fax, the missed referral, the untracked symptom. That invisible space quietly drains nearly $280 billion annually from U.S. healthcare—and worse, it costs lives.
With Medicare’s Enhancing Oncology Model (EOM) now paying practices explicitly for better care coordination, the stakes (and opportunities) have never been higher. But most apps designed to fix this still end up unused—trapped as “shelfware,” frustrating clinicians instead of empowering them.
Here’s the real blueprint for oncology care coordination software that not only gets used, but fundamentally changes outcomes.
Key Takeways
- Coordination chaos isn’t trivial: It’s a $280-billion problem directly tied to patient survival and provider finances.
- Build fewer features—just smarter ones: The right app focuses sharply on referral routing, dynamic care pathways, tumor board collaboration, symptom tracking, and billing support.
- Integration and adoption beat innovation: If clinicians and patients don’t love your tool, it’s shelfware. Embed deeply in workflows, empower nurse champions, and close patient feedback loops—or watch your ROI evaporate.
Table of Contents
- The $280-Billion Coordination Hole No One Owns
- Dissecting a Best-in-Class Oncology Coordination App
- Plugging Into the Oncology Tech Jungle—Without Torching Dev Cycles
- Compliance Minefields: HIPAA, Cures Act, ePA & State Mandates
- Proving ROI: From Value-Based Care Scores to Payer-Side Reimbursements
- Clinician & Patient Adoption Playbook
- Future-Proofing: Genomics at the Point of Care, Wearables for PROs & LLM Copilots
The $280-Billion Coordination Hole No One Owns
Cancer care doesn’t break down in the chemo chair—it breaks down in the hand-offs. Faxed referrals, voicemail tag, a missing ride to infusion: the “in-between” is where money (and lives) quietly evaporate.
Hidden Costs of Dropped Balls
- Avoidable readmissions: Medicare shelled out $15.2B on adult readmissions in 2018; watchdog reviews peg ≈ 27% of those stays as preventable—$4B a year blamed on botched transitions and discharge delays.
- Treatment delays = mortality: A BMJ meta-analysis shows every 4-week lag in surgery, chemo, or radiation ups the death risk across seven common cancers. Translation: scheduling chaos is lethal.
Add it up across the oncology continuum and the tab nudges $280 B. That’s not “oops money”—that’s a national line-item.
CMS Fires the Starter Pistol: The Enhancing Oncology Model (EOM)
Launched July 1 2023 and running through June 2030, EOM is Medicare’s loudest wake-up call yet:
| What Practices Get | What They Must Do |
| $110 per patient per month (starting Jan 2025) | 24/7 clinician access & patient navigation |
| Performance-based upside | Screen + act on social determinants (ride, housing, food) |
| Five-year runway to refine workflows | Hit quality & cost targets—or repay CMS |
The message is clear: coordinate or pay twice—once in penalties, once in readmissions.
Failed coordination isn’t a rounding error; it’s a multi-billion-dollar bleed that worsens survival odds. With EOM literally paying clinics to navigate, triage, and follow up, the only question left is: Will your tech stack stop the leak—or keep the fax machine humming?
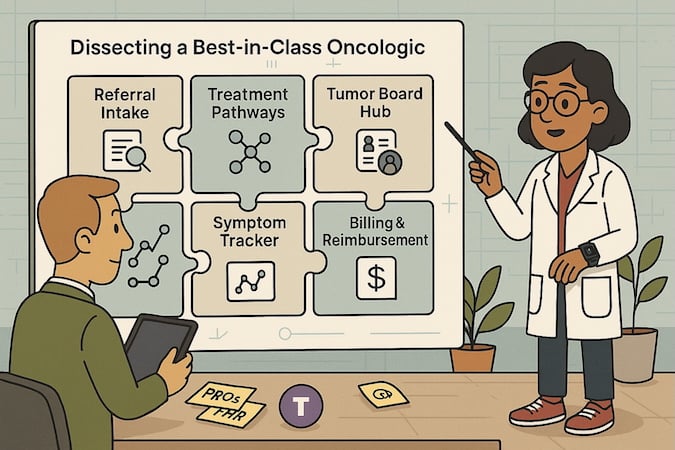
Dissecting a Best-in-Class Oncology Coordination App
You don’t need 50 features. You need the right five—built to untangle oncology’s messiest workflows.
Below is the blueprint that separates shelfware from mission-critical. Whether you’re building from scratch or stitching into an existing EHR stack, these are the modules that actually move the needle.
Smart Referral Intake
No more paper trails or clerical roulette. A well-built intake module auto-prioritizes new cases by diagnosis severity, flags missing labs, and routes to the right care team based on location, insurance, and modality (e.g., med onc vs rad onc).
Bonus: Plug in NLP to scan incoming PDFs for staging info—manual triage is a time bomb.
Dynamic Treatment Pathways
Baking NCCN guidelines directly into workflows isn’t just helpful—it’s required to scale safely. A dynamic pathway engine adapts based on staging, biomarkers, comorbidities, and even patient preference (e.g., hospice vs aggressive care).
When it works right, care teams stop improvising—and start optimizing.
Tumor Board Collaboration Hub
Tumor boards shouldn’t be a calendar invite with 14 attachments. This module enables asynchronous case prep, live review with markup tools, and structured output that feeds back into the care plan.
Essential for: multisite networks, community/rural + academic partnerships, and anytime someone says “we use OneDrive and email.”
Symptom Tracking + PROs
Patients are the real frontline here. A solid coordination app collects daily PROs (pain, fatigue, appetite, nausea) and triggers red-flag alerts that triage nurses can act on fast—before it becomes an ER visit.
Pro tip: Add wearable sync (e.g., for HR, step count) to catch silent deterioration.
Revenue & Billing Assist
Coordination without reimbursement is philanthropy. A best-in-class app streamlines ePA and prior auth processes, pulls CPT codes for team-based care (like navigation), and generates audit-proof documentation for care coordination fees.
Think: less time fighting denials, more time fighting tumors.
Modular vs. Monolithic: Choose Your Battles
Finally, architecture matters. Monolithic apps often trap you in tech debt and change-order hell. Modular builds let you replace or upgrade pieces (like PROs or billing) without breaking everything else.
If it can’t flex with your future EHR upgrades, it’s not scalable.
Plugging Into the Oncology Tech Jungle—Without Torching Dev Cycles
Here’s the thing no one tells you until you’re three sprints deep and hemorrhaging dev hours: building a great coordination app is only half the battle. The other half? Making it talk to the monsters—Epic Beacon, Varian Aria, Cerner PowerChart Oncology, Elekta Mosaiq, and whatever legacy scheduling Frankenstein the front desk still clings to.
Let’s decode the three-headed beast of oncology interoperability.
The Big Three Data Standards: Choose Your Poison
FHIR Bulk Export
The speed demon. Great for tumor board dashboards, population analytics, or ML pipelines that need all the data, now.
- Fast: Multi-million record exports in minutes during 2023 benchmarks.
- Secure(ish): Granular OAuth scopes + signed URLs = low blast radius—but one bad scope and you’re spraying patient data to S3 like a firehose.
- Dev Needs: A FHIR server that supports $export, plus mCODE mapping if you’re smart.
- Best For: Tumor board prep, analytics dashboards, anything asynchronous.
Proof: Corewell Health slashed tumor board prep from 25 to 9.5 hours using FHIR-based automation—freeing 800+ clinician hours a year.
HL7 v2 Messages
Old-school but still undefeated in real-time responsiveness.
- Responsive: Second-level latency on ADT or lab alerts.
- Risky: Demographics get blasted with every segment. TLS is DIY—expect VPNs or MLS tunnels.
- Painful: Every feed’s a snowflake. Mapping ADT/ORU/billing into a coherent cancer episode = weeks of sweat.
- Best For: Live workflows—chemo chair scheduling, bedside alerts, census updates.
C-CDA Documents
The legacy workhorse. Easy to share. Ugly to parse. Misleadingly called “interoperable.”
- Slow: Nightly or on-demand; parsing = seconds-to-minutes latency.
- Overkill: Each doc is a PHI-dense XML novella.
- Messy: Need XSLT or NLP to extract useful staging/treatment data.
- Best For: Referral packets or human review, not workflow automation.
Why This Suddenly Matters to Your Boss
- OIS market is ballooning to $3.2B by 2025, with 7%+ CAGR as cancer centers chase quality bonuses and prep for AI workflows.
- Healthcare interoperability spend hits $4.5B in 2025—projected to triple by 2034. Translation: the fax apocalypse is (finally) being budgeted out.
How to Pick Your Stack
- Need it live? Go HL7 v2—but budget for mapping misery.
- Need it all? Go FHIR Bulk—lock scopes tight and encrypt object stores.
- Need a one-off dump? C-CDA works—just don’t call it integration.
ROI Pitch to the Exec Team
- FHIR Bulk = fewer tumor-board prep hours
- HL7 = fewer missed infusion starts
- C-CDA = audit-ready completeness (with a side of eye strain)
If your app doesn’t play nice with at least two of these, you’re not coordinating care—you’re just adding another inbox.
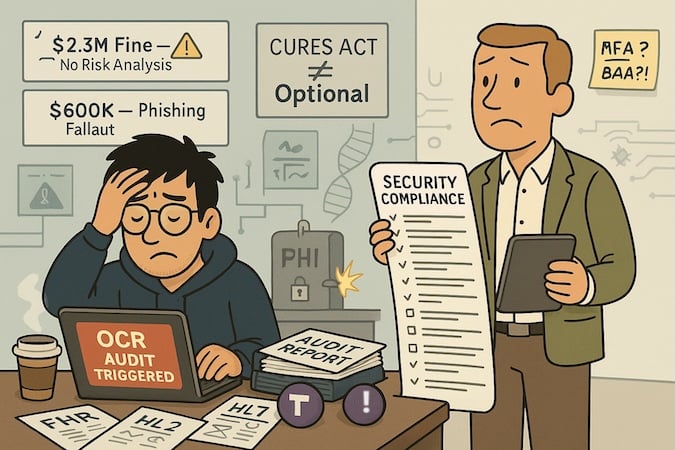
Compliance Minefields: HIPAA, Cures Act, ePA & State Mandates
It’s not just about building a “secure” app—it’s about not waking up to an OCR press release with your name in the fine print.
The world of oncology care coordination sits at a brutal crossroads: rich in PHI, connected to dozens of outside systems, and now under dual pressure from HIPAA and the 21st Century Cures Act. Translation? Screw up once, and you’ll need more than an IT consultant—you’ll need lawyers, auditors, and a 5-year integrity agreement.
Case #1 — 21st Century Oncology: $2.3M HIPAA Fine & Corporate Integrity Agreement
A cyberattack exposed the PHI of 2.2 million patients. OCR found the group never conducted a formal risk analysis, failed to secure their systems, lacked business associate agreements, and didn’t audit system activity.
The cost? $2.3 million + a multi-year government monitoring program.
The kicker? The PHI leak wasn’t due to a new, flashy AI feature—it was basic due diligence left undone.
Case #2 — PIH Health (California): $600K Fine for Phishing Fallout
A staff member clicked a bad link. Nearly 190,000 patient records (labs, diagnoses, demographics) were exposed. OCR called out inadequate security controls and mandated a two-year overhaul—risk assessments, new policies, and retraining.
If you think MFA is “nice to have,” read that again.
The New Sheriff: 21st Century Cures Act & Info Blocking
Even if your app isn’t storing data—it might still be blocking it.
Under the Cures Act, health IT vendors and networks can be fined up to $1 million per violation for “information blocking,” i.e., intentionally making it hard to share health data. Think: refusing FHIR access to tumor-board apps, stalling data exchange, or hiding behind vague API excuses.
There haven’t been oncology-specific fines yet—but given how central coordination apps are becoming, they’re likely next in line.
What This Means for Coordination Apps
If you’re storing PHI, you need:
- End-to-end encryption
- Audit trails
- Signed BAAs
- Real risk assessments (not just checklists)
If you’re routing PHI, you need:
- API transparency
- Standards-based data sharing (FHIR, HL7)
- Role-based access & minimum necessary filters
Security and compliance aren’t features—they’re launch requirements. If your coordination app isn’t hardened, auditable, and built to share data under FHIR, you’re not just at risk of fines—you’re in violation before go-live. And OCR doesn’t care if you’re a startup or a system. They fine just the same.
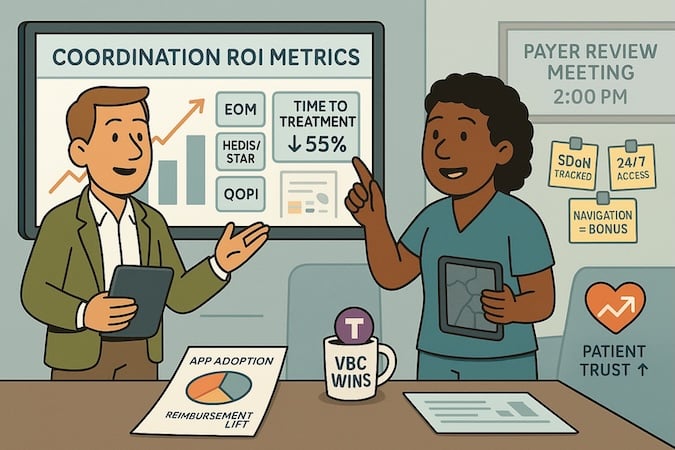
Proving ROI: From Value-Based Care Scores to Payer-Side Reimbursements
Care coordination doesn’t just feel better—it pays better. The right oncology coordination platform can cut costly delays, reduce ER usage, and unlock bonus payments tied to metrics that actually matter to payers and execs.
Let’s map the tech to the dollars.
Value-Based Scorecards: Where Apps Start to Shine
Effective coordination tools move the needle on the very metrics that Medicare and commercial payers track like hawks:
- EOM (Enhancing Oncology Model):
- Timely therapy initiation
- Patient navigation documentation
- 24/7 access + SDoH interventions
- HEDIS/STAR:
- Follow-up after hospitalizations
- Symptom and side-effect management
- Patient experience scores
- OCM legacy (and its carryover in payer contracts):
- Hospice utilization
- Avoidable hospital admissions
- Patient-reported outcomes (PROs)
- QOPI (Quality Oncology Practice Initiative):
- Documentation quality
- Treatment planning and staging consistency
In other words: good coordination doesn’t just reduce chaos—it drives actual reimbursement upside.
Case in Point: XpediteMD at a Nevada Health System
Use case: Coordinating care for breast cancer patients from biopsy to treatment, with a focus on Medicare Advantage members.
Result:
- Median time-to-treatment (TTT) dropped from 74 to 33 days—a 55% reduction (p < .0001)
- Hit key survival-linked threshold: under 30 days to therapy initiation
Let that sink in—41 fewer days of delay, with a corresponding boost in projected survival. Literature shows each 30-day delay correlates with a 9–10% drop in long-term survival, so the impact here is both clinical and financial.
Faster initiation also likely reduces ER visits from unmanaged symptoms or disease progression (though the study didn’t quantify that).
Bonus: The Patient Experience Bump
In a randomized trial at UC Davis, patients using the Personal Health Network (PHN) app with nurse coordination reported:
- Better communication with clinicians
- Lower anxiety during chemo
- Easier symptom tracking
While it lacked hard utilization outcomes, the takeaway is clear: mobile coordination + human support builds trust, keeps patients engaged, and probably improves schedule adherence upstream.
What to Say in the Boardroom
Want to justify your budget?
- “We can reduce treatment delays by 40+ days, which boosts survival odds and likely trims avoidable ER use.”
- “We’re targeting EOM bonuses by hardwiring navigation and SDoH tracking.”
- “The patient app isn’t fluff—it smooths workflows that prevent chemo reschedules and improves HEDIS scores.”
The ROI isn’t speculative anymore. Coordination apps are shortening time-to-treatment, supporting value-based reimbursement, and giving clinicians the tools to actually track what they’re accountable for. The bonus? Patients feel it, too.
Clinician & Patient Adoption Playbook
Let’s be blunt: your app could win a design award, but if nurses hate it and patients ghost it, it’s shelfware.
The biggest risk to any oncology care coordination tool isn’t the tech—it’s no one using it. Adoption isn’t just a feature; it’s a survival metric. Here’s how to crack it.
1. Make Nurses the Champions—Formally, Not Just Figuratively
The most successful apps don’t rely on “super-users.” They institutionalize the nurse champion role—think: dedicated navigators with clear job descriptions, training, and time allocation.
Proof it works: In the CAPRI trial, oncology nurse navigators using a digital remote monitoring platform significantly improved outcomes.
- More NN (nurse navigator) interactions → fewer ER visits
- Proactive nurse advice → shorter hospital stays
- Oncologist referrals → appropriately longer stays for complex cases
This wasn’t an app replacing humans—it was an app that amplified clinical judgment.
Pro tip: Build features that support nurse workflows: templated advice modules, escalations with one-click alerts, and sentiment tracking tied to patient-reported symptoms.
2. Design Patient Tools That Do Something (Not Just Log Data)
ePROs (electronic patient-reported outcomes) aren’t fluff—they’re clinically validated tools that improve outcomes when done right. But they only work if patients actually use them.
Example: The Varian Noona app color-codes symptom severity, sends auto-questionnaires at key treatment windows, and supports photo uploads.
- Result? Chemo reviews dropped from 21 to 7 minutes.
- Patients felt more in control, preferred the app over calls, and flagged symptoms earlier.
Carevive takes it further with algorithm-driven care plans that integrate ePROs + EHR + evidence-based guidelines, slashing care plan build time from 90 to 10 minutes.
Design rules to live by:
- Close the loop: If patients report something, the system must respond—automated tips, nurse alerts, or at least a “we got it” ping.
- Personalize content to diagnosis, treatment stage, and patient goals.
- Design for everyone: Simple UIs, emoji-scale symptom sliders, language access, and offline functionality aren’t nice-to-haves.
3. Integrate or Die: If It’s Not in the Workflow, It Won’t Work
No EHR integration = extra clicks = guaranteed clinician resistance.
- One study found nurses abandoned a PRO tool simply because it wasn’t inside their EHR.
- At AHCI, UpToDate’s patient platform succeeded because it was baked into Epic, auto-triggered education, and matched clinical decision support tools the team already trusted.
- UCSF & Color Health used an AI copilot to review patient records—what used to take days was down to 5 minutes, quadrupling identification of missing labs.
Want to sell it internally? Run a process mining analysis before and after launch to show time saved, steps eliminated, or throughput gains.
TL;DR Adoption Blueprint
| Stakeholder | What Works | Built-In Feature Ideas |
| Nurses | Champion model + templated workflows | Advice library, nurse dashboard, 1-click escalation |
| Patients | Symptom triage + instant feedback | Emoji symptom sliders, auto-responses, photo uploads |
| Clinicians | Deep EHR integration + AI shortcuts | Triggered alerts, smart summary cards, CDS hooks |
If you want sustained adoption, build apps that augment humans, not replace them. That means empowering nurses as drivers, closing feedback loops for patients, and embedding utility deep into the workflows clinicians already use. Don’t ask people to change behavior—build around what they already do, and make it better.
Future-Proofing: Genomics at the Point of Care, Wearables for PROs & LLM Copilots
Let’s be honest: most “cutting-edge” apps are outdated by the time they survive procurement.
That’s why today’s oncology coordination tools need to be built for tomorrow’s reality—where liquid biopsies, ambient symptom monitoring, and AI copilots aren’t “innovations,” they’re expectations. If your platform can’t keep up, your workflows (and outcomes) will fall behind.
1. Genomics at the Point of Care
Precision oncology isn’t a buzzword—it’s the new normal. Platforms like FoundationOne, Guardant, and Tempus now deliver real-time mutation profiling that should inform treatment decisions at the moment of diagnosis, not three weeks later.
The trap: Many coordination apps don’t ingest or surface genomic data in actionable ways, forcing clinicians to swivel between portals.
The fix:
- Integrate structured genomic data directly into patient timelines
- Flag targetable mutations in treatment plans
- Auto-trigger pathways (e.g., MSI-high = prompt for ICI eligibility)
The future isn’t “can we support genomic data”—it’s how fast can we act on it.
2. Wearables as Passive PRO Engines
Why wait for the patient to say they feel worse when their resting HR and step count already told you two days ago?
Wearables (Apple Watch, Fitbit, Withings, etc.) are already tracking fatigue, mobility, and sleep quality—all of which correlate with treatment tolerance and QOL.
- A 2024 trial from UCSF showed that integrating passive wearable data into a symptom triage algorithm improved early intervention for patients on oral chemotherapy.
Your app should:
- Sync with consumer-grade devices (no one wants another login)
- Normalize thresholds based on treatment type (fatigue post-chemo ≠ same as baseline)
- Triage passively collected data alongside ePROs to reduce alert fatigue
Bonus: Wearables help bridge the digital divide—some older patients are more compliant with step goals than daily app check-ins.
3. LLM Copilots for Clinical Speed & Sanity
If ChatGPT can write SOAP notes and summarize radiology reports, why are oncology nurses still copying labs into spreadsheets?
AI copilots are already embedded into EHRs like Epic and Cerner. The best coordination platforms will:
- Auto-flag missing pathology or imaging
- Summarize intake forms for tumor boards
- Draft templated care plans from structured data
UCSF’s AI copilot (built with Color Health + OpenAI) reduced chart review from hours to minutes, quadrupled data completeness, and accelerated plan creation.
LLMs aren’t just buzz—they’re a workflow multiplier. When baked into the app layer, they give clinical teams time back and eliminate low-value tasks.
Build Modular or Rebuild Later
Tech shifts fast. If your architecture doesn’t support plug-and-play evolution—genomics today, AI summary tomorrow—you’re building an expiration date.
- Modular platforms let you slot in new data streams and triage layers without a full rework
- Monolithic builds? Good luck getting that approval again in 18 months
Future-proofing isn’t about chasing shiny objects. It’s about building coordination infrastructure that evolves with oncology itself.
- Genomics will be expected.
- Wearables will be normal.
- AI will be invisible—but essential.
If your coordination app isn’t architected to grow with these trends, you’re not building a product—you’re building technical debt.
Frequently Asked Questions
Whats the biggest overlooked barrier to oncology app adoption
Lack of formal roles like Nurse Champions. Without protected time and recognition, even the best digital tools are often left unused or quickly abandoned.
How do I quickly evaluate if my app has a shelfware problem?
Check login frequency. If daily clinician usage dips below 60% after launch month, your app isn’t essential—it’s optional, and that’s a death knell.
Which oncology-specific interoperability standard should my tech team master first?
FHIR Bulk Data Export, hands down. It’s becoming the backbone of rapid tumor board data integration and large-scale analytics in oncology.
We're a smaller oncology practice - how realistic is AI for our coordination app?
Surprisingly realistic. Many EHR vendors (Epic, Cerner) and emerging oncology platforms now include integrated AI tools, reducing upfront cost and complexity. Focus first on practical use-cases like summarizing patient history and flagging missing labs.
How can we prove our coordination app actually saves money?
Use “process mining” to quantify pre/post app implementation improvements—like time saved per task or reduced treatment delays—to directly correlate adoption with financial and operational ROI.
What common security oversight could put my oncology app at risk?
Not conducting a real, documented security risk analysis. OCR fines regularly hammer practices for skipping this basic step—no matter how secure your app feels.