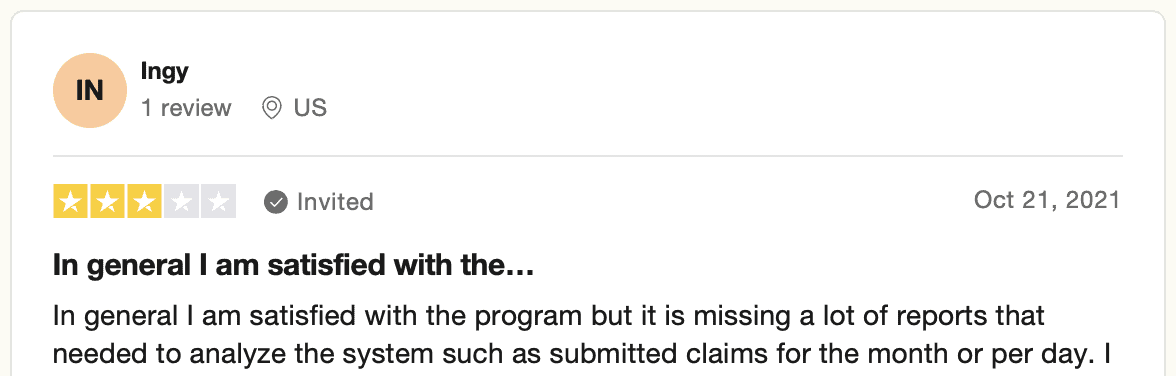
Today, it’s hard to imagine a medical facility managing its revenue cycle without a software system. I bet medical billers and coders — the central pillars holding up the revenue cycle at any healthcare organization — would have much to say about the efficiency of these systems. In fact, they do:
 Images credit: Trustpilot (all image rights belong to Trustpilot Inc.)
Images credit: Trustpilot (all image rights belong to Trustpilot Inc.)
Yes, software can be hard, and we can’t always get what we want. But if we try to introduce artificial intelligence to help billers and coders, we may get what we need.
AI medical coding and billing come to the rescue. That’s going to be our topic of discussion today. Let’s talk through all the whys and hows of using AI software to improve revenue cycle management.
I bet you sense the timing for such AI innovations is ripe; you just need details before you dip a toe in the water.
Top Takeaways:
- Computer-assisted coding and billing in medicine work wonders. Companies enjoy higher revenue due to faster, more accurate, and more comprehensive coding and streamlined revenue cycle management. Scaling up becomes available almost immediately with AI-assisted medical coding, giving medical facilities the ability to handle larger volumes efficiently. The results are viewed positively by healthcare members and hospital administrators alike.
- We can apply different AI technologies to empower medical coders and billers. However, natural language processing seems to be the most promising AI medical billing solution. This technology helps hospitals save money and improve productivity by automating complex coding tasks. Additionally, it reduces the monthly burden on human coders and billers, allowing them to focus on supervisory roles and ensuring accuracy.
- Machine learning algorithms do not replace human coders and billers. Instead, they elevate them to a supervising position, providing critical oversight while using AI for medical billing to handle routine tasks. By integrating these technologies, hospitals can better manage their revenue cycles, making informed decisions based on accurate data. This overall improvement leads to an enhanced general understanding of financial positions within healthcare organizations.
Table of Contents:
- Traditional Medical Billing & Coding Process Flow
- Overview of Paper-Based Claim-to-Payment Chase
- AI’s Impact on Medical Billing and Coding
- Possible Challenges Faced by Artificial Intelligence in Medical Coding and Billing
- The Future of AI in Medical Coding and Billing
- Specific Applications of AI in Medical Billing and Coding
- How Topflight Can Help
Traditional Medical Billing & Coding Process Flow
On the face of it, medical billing and coding look pretty straightforward. As providers, we need to set in code all healthcare services received by the patient and bill them to the payer.
We must cross-reference all diagnoses, treatments, examinations, etc., to accurately describe provided services and maximize the revenue potential.
Of course, the devil is in the details. Coders and billers (to a greater degree) must handle quite a few things to keep the revenue cycle afloat. Medical billers play key parts at the beginning of patient interactions and towards the end, while coders hum away in the middle of the process.
As you know, in many healthcare organizations, medical billing and coding can be carried out by the same person. However, as we continue to explore billers’ and coders’ responsibilities side by side, you’ll notice that coding, in particular, is perfect for automation. AI and medical coding are destined for each other.
Also Read: Healthcare App Development Guide: Everything You Need to Know
Medical billing
Let’s quickly recap medical billing tasks. As we go through the list, we’re trying to identify the most laborious, repetitive tasks we can pass on to artificial intelligence.
But before we go any further, here’s a brief disclaimer: artificial intelligence medical billing does not imply we don’t need human talent anymore.
What do billers do?
- Handle correspondence: emails, messages, voice mails, and phone calls (to answer patients’ and insurance companies’ questions)
They often use task management systems to keep tabs on these activities. We could apply AI to sort all their tasks according to their impact on a business’s revenue. Therefore, an optimal scenario is to find a CRM, ERP, or task management platform with AI capabilities.
- Capture patient data, for example, demographics, payment info
You’re right to assume that this task is the front desk’s responsibility. However, billers sometimes have to check and correct any data inconsistency in patient documentation. This data typically gets into the system manually. We could develop a natural language processing app to ease data entry.
- Verify patient eligibility and benefits
For many billers, that still means hanging on the line with an insurance carrier or a clearing house. Ideally, AI medical billing software connects with the corresponding system on the payer’s side to run patient eligibility verification.
- Add charges into a practice system (from a split fee or superbill), or copy this information from an EHR to some other practice management/billing software.
Read more about EHR in medical billing in our blog.
An AI-assisted practice management system can automatically pull the required data as necessary, removing the need for manual work.
- Communicate with providers (some things may be missing: charges, diagnoses, modifier confirmations — anything necessary for drafting a claim and sending it to an insurance company)
Again, AI in medical billing can absolutely handle that and automatically pull data from EHRs and other platforms, asking doctors to verify edge cases.
- Send claims to a clearing house/payer and track their progress
This is definitely a no-brainer area for applying machine learning for medical billing. Why make people click buttons when an AI can automatically send fully prepared claims as soon as they are ready and then monitor the responses based on a set turnaround time for reimbursement.
- Handle rejections from a clearing house to ensure the claims are processed and passed onto insurance carriers. Includes preparation of reconsiderations and appeals.
This is an area for the next potential breakthrough of artificial intelligence in medical billing. The billing software will need to rely on deep learning for the algos to continue learning from errors. And the outcome will be more cleared claims in the future.
- Manage received checks and payments (mailing them to a bank or preparing them for the management)
Electronic payments should take care of that without any AI assistance. However, management might appreciate automatic revenue forecasts based on completed, missing, and delayed payments. Medical billing automation can set you apart from the competition.
Read more on healthcare payment system integration
Artificial intelligence and medical coding continue to evolve, with each new edition of software and technology improvements offering more nuanced functionalities. For instance, consider this surprising use case: obtaining a coding certificate has become increasingly accessible through online courses powered by AI, making it easier for professionals to stay up-to-date with the latest advancements.
Read more on medical billing software development
Medical coding
What about coders? They have somewhat fewer tasks. Nevertheless, their work is very stressful as it requires complete concentration. And it’s pretty much repetitive and manual in nature.
- Assign ICD-10 codes to all performed services on a patient health record
Finding an appropriate code in the sea of 14,400+ codes is not exactly an easy feat. And ICD-11 introduces 4x more codes.
But it’s not only about the quantity. Coders must also attribute the most appropriate codes: every diagnosis or treatment can be coded differently.
Of course, that’s the best target for applying machine learning in medical coding. Algorithms can learn from approved claims and identify patterns for distributing the most applicable and revenue-efficient codes.
- Manage appeals if auditors reject certain codes or insist on adding, removing, or replacing some other codes in a chart
That’s the most tricky part of coding, and since AI in medical coding relies on past experience, we get yet another confirmation for applying this technology. Machines can untangle the mess of cross-coding when dealing with clinically supported conditions with casual relationships.
Overview of Paper-Based Claim-to-Payment Chase
I honestly thought to include this section here just as a reverence for days gone by when providers had to deal with paper and mail. It turns out, as of 2017, 77% of physician practices still relied on paper-backed processes for billing.
I couldn’t find more recent stats, but even if the rate is closer to 40-50%, that’s still a lot. If you’re a healthcare provider, you know it’s a nightmare for the healthcare industry.
- Collect data for claims
- Prepare and submit claims
- Work through denials
- Register payments
And all of that manually, using mail delivery services. When carriers have strict deadlines for submitting claims, such a paper-based workflow is a disaster.
AI driven medical billing systems, like GaleAI, offer a transformative solution by automating these time-consuming tasks, enabling healthcare providers to order and process claims with greater speed and accuracy, significantly reducing the need for manual intervention.
And note that we’re only discussing the switch to digital workflows. AI and ML-driven data processing is the next step after digitization.
Again, if you’re a provider stuck with paper workflows, you should absolutely check out solutions like GaleAI. I kid you not; you’ll be impressed by the new efficiency of AI-powered coding and billing. This is a must for effective revenue cycle management in the 21 century.
Artificial intelligence in healthcare has already set out on a quiet revolution. The ability to swiftly purchase and integrate AI solutions is making a significant impact on how artificial intelligence for medical billing is approached, driving productivity and accuracy to new heights.
AI’s Impact on Medical Billing and Coding
AI isn’t just creeping into healthcare admin—it’s taking a scalpel to inefficiencies and suturing up revenue leaks. Here’s how artificial intelligence is transforming medical billing and coding in 2025.
Automation in Medical Coding with AI
AI in medical coding now means much more than just automation. It’s about end-to-end transformation.
For starters, AI can flawlessly parse through patient records, doctor notes, and other documentation—any digital format is fair game. Even scans and professional medical imagery are becoming usable inputs when paired with OCR technology (optical character recognition). That means even handwritten notes can feed into machine learning algorithms for training and deployment.
Real-time feedback is a common manifestation: AI highlights questionable codes and suggests replacements while coders work. Alternatively, batch processing can occur post-factum, where AI-assisted medical coding tools scan charts, forward clean claims to billing, and flag edge cases needing review.
Doctors also benefit. If they input notes electronically, AI can suggest codes on the fly, building out Superbills in real time. This makes AI a hands-on assistant—not a passive observer.
AI-Driven Improved Accuracy in Medical Coding
Accuracy is where AI shines hardest—especially in preventing under-coding and capturing modifiers and severity levels that humans might overlook.
Using Natural Language Processing (NLP) and Deep Neural Networks, AI helps ensure more accurate code attribution, reducing denied claims and revenue leakage. ML tools assist coders in spotting codes they might otherwise miss, helping providers get reimbursed for every service delivered.
Plus, AI can train new staff by showing them patterns from past correct and incorrect coding instances—bringing junior coders up to speed faster.
Increased Efficiency in Medical Billing with AI
AI never sleeps, doesn’t burn out, and doesn’t need coffee breaks.
In billing workflows, AI algorithms validate insurance eligibility, automate claims submission, and track claim status. Some providers are even experimenting with voice input for billers, letting them dictate instead of type.
AI also assists in claims processing by scanning health records and insurance cards. It prioritizes billers’ workloads based on impact to revenue and processes more charts in less time—allowing organizations to scale without hiring at the same rate.
With AI, Superbills get ready faster, and the entire cycle from service to payment speeds up dramatically.
Cost Reduction through AI in Medical Coding & Billing
By offloading the routine grunt work to AI, healthcare organizations can lower operating costs without compromising quality.
Coders and billers can be promoted into supervisory roles, overseeing exception cases flagged by the AI. On the auditing side, fewer errors also mean less need for deep post-submission review.
Because AI runs 24/7 in the cloud, the only ceiling becomes your cloud provider’s capacity—which is both affordable and highly scalable.
It’s not about replacing people—it’s about elevating them.
Enhanced Data Analysis with AI in Healthcare Coding
Beyond automation and speed, artificial intelligence for medical coding also unlocks insights from massive volumes of billing data.
AI models trained on rejected claims can predict where things might go wrong in the future—highlighting high-risk cases and enabling proactive correction. This keeps the revenue cycle clean and compliant.
For billers and payers alike, these insights enable tighter feedback loops, smarter workflows, and ultimately complete claims that capture the full scope of treatment and diagnosis procedures.
Also Read: App development Costs: The Ultimate Guide
Possible Challenges Faced by Artificial Intelligence in Medical Coding and Billing
What about the challenges healthcare organizations may face when applying machine learning in medical billing and coding?
HIPAA compliance
Medical software dealing with patient data must be secure and HIPAA compliant. So it goes without saying that AI-driven medical billing and coding applications that process critical financial and health data must meet these standards.
Also Read: HIPAA Compliant App Development Guide
Different data formats
The ubiquitous interchangeability. Businesses still work with software systems that output data in various formats, which makes it harder to sync. Even if we want to create an AI application to automate coding and billing for our own organization, we have to account for sharing this data with third parties, who may use different tools.
Integrations with carriers
Besides varying data formats, we also need to ensure our insurance partners can seamlessly plug into our automation workflow. There are two ways to address that, either integrate our AI systems with an insurance carrier’s APIs or provide them with our own APIs and tools for syncing claims.
Staff pushback
Billers and coders may be under the impression that a company is looking to replace its jobs when undertaking AI implementation. It takes a substantial effort to educate them and explain how their upgraded daily workflows will benefit the business.
Data training
Super intelligent billing and coding robots don’t come out of nowhere. Access to historical data on coded patient charts and processed claims (both rejected and approved) is critical for algorithms training.
Continuous learning
Machine learning algos will need to continue learning based on new data and internal audits. That means we must set up a neural network capable of analyzing new data, auditor feedback, and historical data.
Changing standards
Most healthcare organizations still code according to the ICD-10 standard. However, ICD-11 has been in effect since January 1, 2022, and a slow transition to the new format has already started. ICD-11 has more codes and other changes allowing for even more accurate coding.
The Future of AI in Medical Coding and Billing
The future of artificial intelligence in medical coding and billing isn’t just “bright”—it’s actively being coded into existence. While early tools focused on speed and error reduction, we’re now entering a new phase of evolution: prediction, personalization, and automation that doesn’t replace humans—it elevates them.
Let’s break it down.
AI Will Likely Augment, Not Replace, Human Coders
Despite the hype, AI won’t be putting seasoned coders out of a job anytime soon—and that’s a good thing.
Instead, we’ll see AI acting as a highly skilled assistant:
-
Increased accuracy and efficiency: AI medical coding software will continue to offer real-time predictions and suggestions that boost productivity for human coders.
-
Reduction in human error: Complex code mappings and documentation inconsistencies are areas where AI thrives, reducing mistakes that impact reimbursements.
-
Enhanced revenue potential: As shown in the GaleAI case study, AI can surface missed codes and optimize claim submission—resulting in significant revenue gains.
But human coders are still the ones reviewing edge cases, validating complex scenarios, and training the AI models themselves. Think co-pilot, not replacement.
AI-Driven Systems Will Become More Sophisticated and Adaptable
We’re heading toward a future where AI systems won’t just react—they’ll anticipate. These capabilities mark the evolution from rule-based tools to AI-powered medical coding systems that are context-aware and built for flexibility in high-stakes environments.
Here’s a glimpse into what’s next:
-
AI-powered medical audits and fraud detection: By analyzing massive datasets, AI can uncover suspicious billing patterns in real time. This isn’t just automation—it’s a new layer of financial protection.
-
Cognitive automation for personalized coding: AI can merge genetic data, medical history, and real-time patient context to proactively assign codes—even before a physician finalizes a diagnosis.
-
AI-driven predictive analytics: Systems will identify bottlenecks in the revenue cycle, such as undercoding or high denial rates, before they become problems—helping providers adjust workflows and improve reimbursement.
In short, AI will increasingly handle edge complexity and adapt dynamically to provider workflows and payer rule changes.
The Healthcare Industry Will Need to Adapt to the Changing Landscape
With AI reshaping the rules, providers, payers, and vendors must evolve too.
-
Conversational billing: Imagine patients interacting with AI chatbots that speak fluent CPT. These systems will be able to explain bills, answer questions, and even manage pre-authorizations—24/7, no hold music required. These systems will be key players in the rise of conversational AI in healthcare, giving patients real-time clarity on charges and helping reduce administrative load.
-
Blockchain-integrated AI: This combo will introduce transparency and trust to a system notoriously lacking both. Smart contracts could validate claims instantly, eliminate duplicates, and accelerate reimbursements. This also enables providers to proactively identify undercoding, one of the most common and costly revenue leakages in healthcare organizations.
-
Training and workflow redesign: Coders, billers, and clinical staff will need training to work alongside AI tools—and healthcare leaders will need to rethink how coding fits into the broader digital health stack.
The big takeaway? Those who embrace AI in medical billing not as a threat, but as a multiplier, will pull ahead in revenue, efficiency, and compliance—while redefining modern healthcare billing practices in the process.
Ultimately, the future of Artificial intelligence (AI) in medical coding will be defined not just by automation, but by how seamlessly it integrates with the evolving workflows of healthcare teams.
Specific Applications of AI in Medical Billing and Coding
Let’s explore where artificial intelligence is making the biggest impact in medical coding and billing today—from smarter documentation to better claim capture and denial reduction.
AI Medical Scribes
AI scribes are transforming clinical workflows by automatically transcribing physician notes and structuring them into code-ready data. Using Natural Language Processing (NLP), these tools minimize manual documentation work while capturing key billing details from patient encounters. This reduces coder fatigue and improves documentation completeness.
AI-powered Claim Processing
AI systems can now handle entire claims pipelines—from interpreting structured/unstructured data to assigning CPT/ICD codes and flagging missing information before submission. These tools reduce claim cycle time, increase accuracy, and free up billing staff for higher-value tasks.
AI-driven Denial Management
Denied claims are a persistent revenue drain. AI tackles this by analyzing historic denial reasons, flagging patterns, and proactively preventing undercoding or mismatched documentation. The result: fewer rejections, faster payment cycles, and more predictable cash flow.
AI for Charge Capture
AI can automatically identify billable services in physician documentation—even if it’s handwritten or embedded in lengthy notes. These systems are essential for improving charge capture rates, reducing revenue leakage, and ensuring providers get paid for every procedure performed.
Our Experience: GaleAI Case Study
Our work with GaleAI showcases the transformative power of AI in healthcare billing.
GaleAI’s development journey, led by Topflight, is a testament to the power of collaboration between industry veterans and cutting-edge technology experts. The project started with digitizing existing paper claims using Optical Character Recognition (OCR), transforming them into usable data for training machine learning algorithms. This foundational step was crucial in building an accurate and efficient AI system capable of handling the complex task of AI assisted medical coding.
Topflight’s approach to developing GaleAI involved meticulous planning and execution, spanning a total of 4,500 hours over 1.5 years. The initial phase focused on creating a Minimum Viable Product (MVP), which took 1,100 hours and was completed in nine months. This MVP served as a prototype, providing valuable insights and feedback that guided subsequent development stages. Topflight’s team ensured that every aspect of the platform, from the user interface to backend algorithms, was optimized for performance and user experience, leveraging advanced medical coding AI tools.
Throughout the process, Topflight emphasized the importance of human supervision in AI automation. While GaleAI automates many aspects of medical coding, human coders were instrumental in training the ML algorithms, validating outputs, and handling edge-case scenarios. This integrated approach not only ensured high accuracy but also fostered trust among users. By leveraging advanced technologies such as Natural Language Processing (NLP) and Deep Neural Networks, GaleAI can autonomously code patient charts, identify missing codes, and even predict potential errors, all while adhering to full HIPAA compliance. The result is a robust, scalable AI healthcare billing solution that significantly enhances productivity and revenue for healthcare providers.
GaleAI’s platform exemplifies how medical coding artificial intelligence can revolutionize the industry:
- Revenue Increase: GaleAI’s ML engine boosts revenue potential for providers by up to 15%.
- Accuracy Improvements: The platform captured 7.9% of codes missed by human coders, translating into significant financial gains—up to $1.14M lost revenue recovered annually.
- Time Savings: AI automation saved coders 97% of their time, improving overall efficiency.
- Full Integration: GaleAI integrates seamlessly with major EHR systems like EPIC and Athena, adhering to FHIR compliance.
- Advanced Technology: Utilizing NLP, Deep Neural Networks, and OCR, GaleAI ensures precise and efficient coding.
- Cross-Platform Accessibility: Available on both web and mobile platforms, it offers innovative features like on-the-go medical notes scanning and instant recognition of handwritten notes.
These accomplishments underline the immense potential of medical coding and AI to transform operations and financial outcomes for healthcare providers.
Topflight’s Experience in this Space
We have solid experience working with various AI automation projects, including natural language processing and imagery recognition. More importantly, we know how to merge this ML/AI development expertise with engaging user interfaces. Because even AI-powered applications operate under human supervision.
We provide full-cycle machine learning development services: from strategy and design to development, testing, and maintenance.
One of the success stories we’re happy to be part of is GaleAI. Their motto is “From medical notes to medical codes in seconds.” GaleAI’s ML engine helps provider increase their revenue potential by up to 15% and saves a great deal of time for coders.
During exuberant tests, a 1-month retrospective audit revealed that the GaleAI platform captured 7.9% of codes missed by human coders, translating into up to $1.14M.
If you have questions about artificial intelligence medical billing or coding and how it can work at your place, reach out.
[This blog was originally published on 2/21/2023 but has been updated with more recent data]
Frequently Asked Questions
How can we switch from paper based claims to fully automated practice?
It’s best to take one step at a time. First, digitize all existing paper claims using OCR (optical character recognition), train ML algos utilizing this data set, and proceed to controlled automation with human supervision. Only after that can we talk about 100% automated medical coding and billing.
How does AI medical coding work?
AI automatically codes all patient charts based on retrospective data analysis or machine learning algorithms enhance coders’ productivity by advising on appropriate/missing codes.
How does AI medical billing work?
Machines automatically collect and verify necessary data, submit claims, and track their status. Human intervention is only required in edge-case scenarios.