Building an automated medical billing system can be quite a challenge. However, more and more medical organizations are willing to throw their hat in the ring. With 10+ years in healthcare automation, Topflight has seen what actually moves claims from “denied” to “paid,” and how to avoid shipping Rube Goldberg workflows that stall cash flow. Because poor billing and coding practices cost U.S. healthcare providers nearly $125 billion each year.
That’s how much is left on the table due to rejected claims, administrative costs, and under-coding. Keep reading if you’re looking for ways to improve the economic lifeblood of your practice. We’ll discuss everything you need to know to step up billing automation.
Top Takeaways
- Automated medical billing processes will help you increase the reimbursement rate and free your staff to work on other critical tasks.
- One trend in optimizing medical coding and billing, offering a measurable impact on the bottom line, is the inclusion of machine learning algorithms for data processing.
- A custom-built automated medical billing platform provides more flexibility in its feature set, perfectly integrates with existing solutions, and can become an additional revenue source on a SaaS model.
Table of Contents
An Overview of the Medical Billing Process
Top 3 Best Medical Billing Solutions
Benefits of Medical Billing Automation
What Can Be Automated in Medical Billing?
Real-World Automation Success Stories
Key Features of Medical Billing Automation
Key Technologies Driving Medical Billing Automation
Medical Billing Automation by Practice Type
Ready-Made vs. Custom Medical Billing Automation Solutions
5 Steps of Medical Billing Automation
- Step 1. Discovery
- Step 2. Functional Proof of Concept
- Step 3. Rapid Prototypin
- Step 4. Development and QA
- Step 5. Deployment and Maintenance
Challenges of Medical Billing Automation
Overcoming Billing Automation Challenges
Topflight’s Medical Billing Technology Stack
Building Custom Medical Billing Automation with Topflight
Cost of Automating Medical Billing
An Overview of the Medical Billing Process
A typical medical billing process is neither too transparent nor streamlined. There are quite a few counterparties and multiple steps involved, and errors are common.
Could medical billing be automated? Yes—start with eligibility checks, coding validation, and claim routing; keep humans on exceptions and payer edge cases.
Usually, a clinic or practice has to clear all the following stages to get paid for its services:
- Collect patient demographics info (for new patients)
- Check patient insurance eligibility
- Assign diagnosis and/or treatment codes (after a patient has seen a specialist)
- Prepare a super bill containing an itemized list of all services provided to a patient
- Prepare and submit a health insurance claim to a clearing house or directly to a payer
- Go through the medical claim adjudication process
- Track the payment from the insurance company
- Settle deductibles, co-insurance, and co-payments as per ERA/EOB
- Bill the patient and track down the payment
Quite a hustle, right? No wonder all that can turn into a mess and cause lost revenue, e.g., in denied claims or underpayments. AI medical coding companies are revolutionizing healthcare by streamlining processes and increasing accuracy in billing and coding.
Top 3 Best Medical Billing Solutions
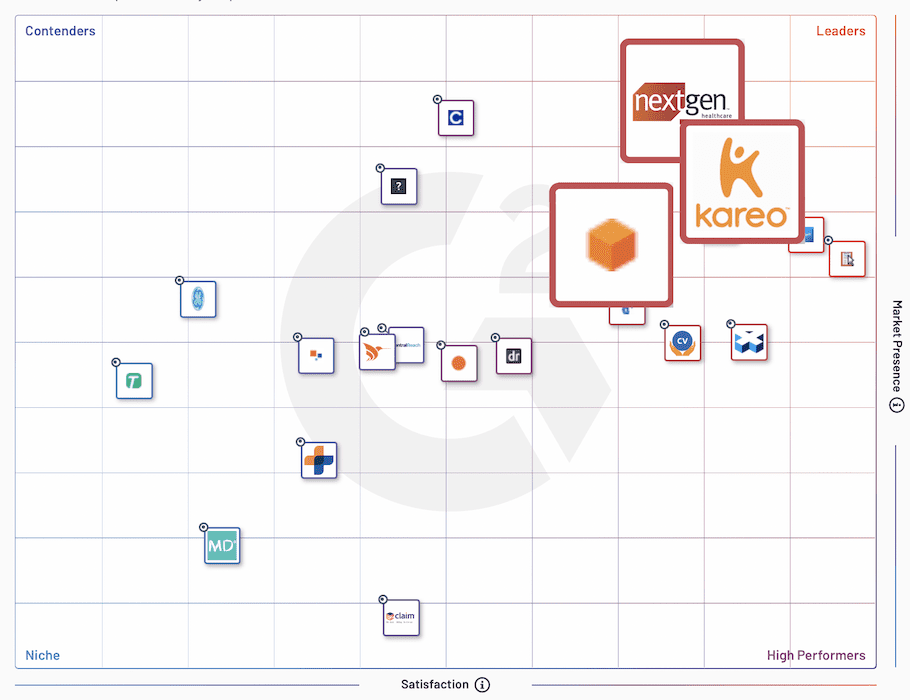
I suggest we review these medical billing platforms, touted as leaders by the top software review site (G2.com): Kareo, Amazon Comprehend Medical, and NextGen.
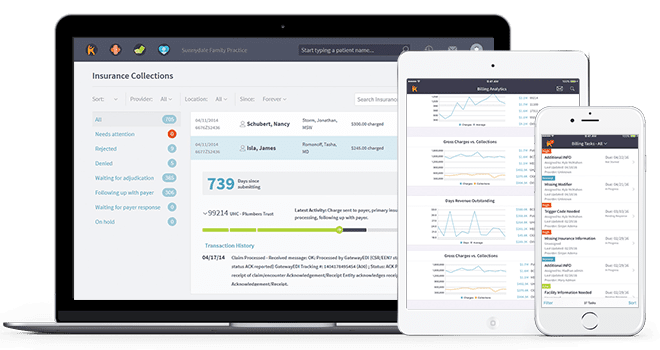
Kareo
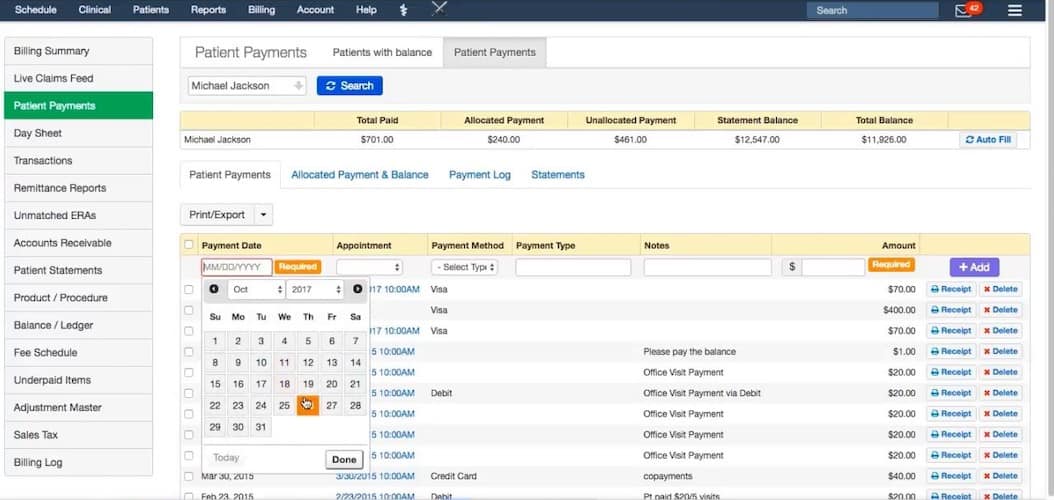
Kareo is a cloud-based clinical and business management platform serving independent practices. Like NextGen, the platform includes much more than pure medical billing and covers all revenue cycle management tasks.
Key features:
- billing analytics
- automated ERA and unapplied payments processing
- claims submission and management
Amazon Comprehend Medical
Amazon Comprehend Medical stands out with its machine learning capabilities. The platform is optimized for automatically extracting information from unstructured medical texts.
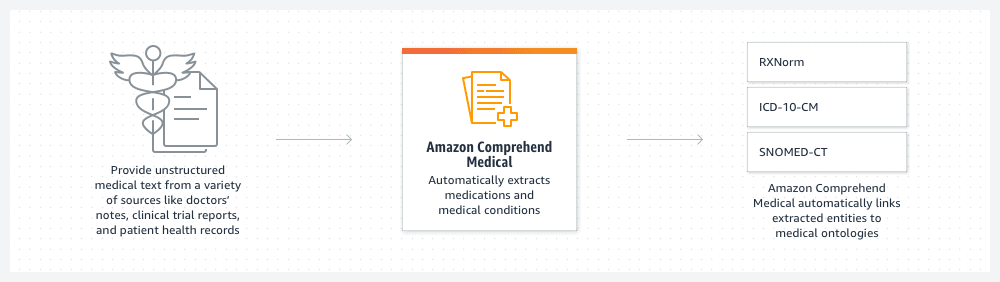
- automated claim capture, validation, and approval workflows
- linking of extracted entities to medical ontologies
- HIPAA-eligible natural language processing
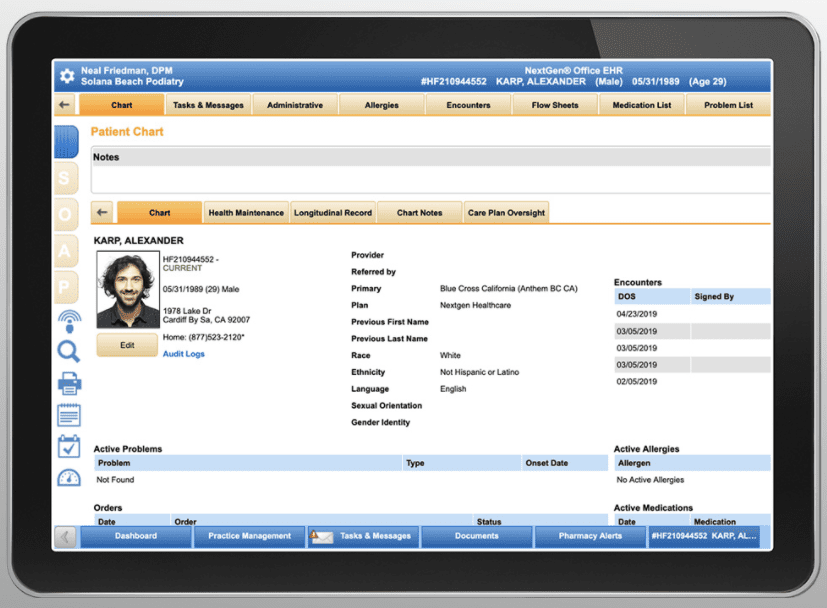
NextGen
NextGen provides out-of-the-box practice management and EHR. The software also allows medical billers to create rules-based charges, manage claims scrubbing and processing, and handle A/R and reporting.
Key features:
- Billing management with support for clinical workflows
- Document management, EM coding, insurance and claims
- Voice recognition, medical templates, patient history
Benefits of Medical Billing Automation
Automation brings about lots of advantages to businesses that embrace it. So let’s list the reasons for automating your medical billing system.
Fewer Human-Caused Errors
Medical coders’ and billers’ routines involve many mundane tasks demanding critical attention to detail. Replacing this manual work with RPA (robotic process automation) helps alleviate potential issues with CPT and diagnostic codes.
As a result, more health insurance claims get paid on the first pass without needing to resubmit or correct data.
Also Read: Healthcare App Development Guide
Automatic Payment Posting and Tracking
A medical billing solution allows billers to submit and track payment requests automatically. If any claims require additional efforts, all personnel will be notified promptly. This helps to streamline and fasten the reimbursement process.
Read more on healthcare payment system integration
You won’t miss submitting claims or appeals (if any).
Remain Compliant
Since an automated healthcare billing system deals with sensitive patient data, it must conform to the HIPAA guidelines and protect patient data.
Also Read: HIPAA Compliant App Development Guide
Reporting
Having all critical data in a healthcare billing and coding solution makes it easy to pull reports aiding decision-making.
Lower Operational Costs
Finally, billing automation in healthcare allows your staff to spend time on other activities that directly affect customer satisfaction and the business’s bottom line.
If you’re curious about the EHR software cost, our blog provides an extensive overview.
Improved Efficiency
Stop burning hours chasing statuses and re-keying data. Automation routes each claim through the same playbook every time—eligibility verification, clean claim submission, work-queue assignment—so cycle times shrink and administrative overhead drops. Fewer handoffs mean fewer stalls, and faster payer responses mean tighter cash flow. In short: let bots handle the repetitive hops while your team handles the exceptions—pragmatic medical billing automation for healthcare providers.
Increased Accuracy
Accuracy isn’t just “no typos”—it’s validated, structured data at every step. AI-powered checks reconcile codes, modifiers, and NPIs against payer rules before electronic claims go out, and cross-reference context from electronic health records to catch mismatches early. Result: fewer downstream reworks and appeals because regulatory requirements and payer nuances are enforced up front, not discovered in denial letters.
Improved Patient Experience
When the back office runs smoothly, patients feel it. Real-time coverage checks surface out-of-pocket estimates before a visit; fewer billing surprises after. Clear statements, timely updates, and easy self-service (inside your practice management system) reduce back-and-forth and phone queues.
Net effect: less friction, faster resolution, and a patient experience that feels intentional—not like they’re debugging your revenue cycle.
What Can Be Automated in Medical Billing?
Automation of healthcare in medical billing applies virtually to all the steps outlined in the first section when describing a medical billing process. If handled manually, these iterations can be pretty time-consuming.
We can roughly divide these activities into:
Data Aggregation and Processing
Our medical billing software should pull all relevant patient medical history from an EHR and other internal systems deployed at a practice. We can even use machine learning algorithms to interpret medical notes and learn doctors’ coding habits.
Read more about EHR in medical billing in our blog.
Claims Management
Once all details have been compiled into a super bill, a claim should be created and submitted electronically. The staff should be able to track its status and monitor automatically handled rejections or denials.
Payment Tracking
Of course, automated medical billing processes integrate tightly with an accounting system to track payments, identify underpayments, etc.
Reporting
Finally, automatic reports help the management with decision-making.
Bottom line: most of this pipeline is automatable if you design for structured inputs, clean handoffs, and exception queues. If you’re asking “How do I automate medical billing and coding?”, start with eligibility APIs and ML-assisted code suggestions, feed clean super bills into EDI (837) pipelines, auto-post ERAs (835), and loop denials back into pre-submission rules. Pilot one service line, measure first-pass yield and days in A/R, and keep humans on edge cases—not the repetitive clicks.
For the end-to-end playbook: eligibility → coding → claims → denials → patient balances, see our guide to healthcare revenue cycle management automation.
Real-World Automation Success Stories
Short, named wins—different levers, same goal: fewer denials, faster cash, less manual lift.
Prior Authorization Automation
When health systems wired prior auth to standards (X12 278 + CAQH CORE rules) and APIs, staff time per case dropped sharply and adjudications landed days sooner. In the Cleveland Clinic study, automated workflows cut waits by 4–11 days across key steps, with marked gains in staff satisfaction and throughput.
Claim Scrubbing and Submission
UW Medical Center overhauled edits and claim flow and saw clean-claim rate rise from 84% → 92%, denials drop by >50%, and days from claim to export fall 33%—proof that disciplined pre-submission automation pays.
Payment Posting Automation
Banks aren’t just vaults—they’re automation partners. One U.S. health system using U.S. Bank’s receivables automation now auto-posts ~75% of lockbox payments; another hospital running Commerce Bank’s healthcare lockbox converted ~99% of paper EOBs to ERAs, accelerating posting while preserving exception control.
AI-Powered Coding Automation
An AI coding platform, GaleAI, deployed across provider workflows identified CPT codes in seconds, lifted revenue up to 15%, surfaced 7.9% more billable codes than human review, and cut coding effort 97%—driven by NLP, OCR, and model-guided suggestions tied to EHR integrations.
Denial Management Systems
Treat denials as a prediction problem, not a cleanup crew. A Fresno, CA health network deployed an AI tool that flags likely denials before submission; prior-auth denials fell 22% and “services not covered” denials fell 18%, freeing 30–35 staff hours/week without adding RCM headcount. The win came from embedding denial intelligence into claim assembly—so fewer appeals are needed later.
Key Features of Medical Billing Automation
Think of these as the non-negotiables of a modern RCM stack: automate the front door and the back office so humans only touch exceptions. Whether you run in-house or with medical billing services, the features below reduce clerical overhead, verify insurance coverage upfront, and turn denials into data you can act on.
Eligibility Verification
Stop playing phone tag. Real-time payer lookups confirm insurance coverage, benefits, and deductibles before the visit, so estimates are accurate and denials don’t start at intake. One click replaces five calls, cutting administrative burdens without adding new ones.
Integration with Existing Systems
Design the seams first. Map data contracts across EHR/PMS/clearinghouse, normalize patient/plan identifiers, and choose an event-driven spine (webhooks/queues) with idempotency. Prefer FHIR for clinical, X12 for claims, and a mediated layer for payer quirks. Build against a sandbox matrix and versioned APIs; add drift monitors on payer responses. Treat integration as a product with SLAs, not a ticket—this is where healthcare RCM automation solutions either fly or leak revenue.
Claim Submission
Ship clean claims on the first pass. Rule-based scrubbing validates ICD-10/CPT, modifiers, and NPI, then generates EDI 837s in batches or on-demand. This is the core that automated medical billing solutions for hospitals must get right—humans focus on edge cases; bots move the rest.
Payment Tracking
Auto-post ERAs (835), map CARC/RARC codes to work queues, and flag underpayments in real time. Cash application accelerates while variance handling becomes a task, not a scavenger hunt. Works whether you run in-house or partner with medical billing services.
Reporting and Analytics
See leaks before they become losses. Track clean-claim rate, first-pass yield, denial reasons by payer, and days in A/R to guide staffing and payer strategy—actionable KPIs, not hindsight. Roll-up views pair nicely with your RCM playbook and the automation solutions already in place.
Key Technologies Driving Medical Billing Automation
These aren’t buzzwords; they’re the engine room. In medical billing automation software development, pick tech that shortens cycle time, improves claim quality, and leaves humans only the judgment calls.
Robotic Process Automation (RPA) in Billing
RPA is your glue for stubborn, no-API steps—payer portals, batch downloads, status checks—scripted, observable, and reversible. Treat bots like teammates: versioned code, audit trails, secrets vaults, and least-privilege access.
- Use for deterministic, UI-stable flows; avoid volatile screens.
- Gate every bot action behind idempotent queues and human-in-the-loop for exceptions.
AI and Machine Learning for Claim Processing
ML shifts work from rework to prevention: pre-submission risk scoring, code/modifier suggestions, and anomaly detection by payer/specialty. Start in shadow mode, then gate edits behind acceptance thresholds; monitor drift like uptime.
- Track lift by cohort (clean-claim rate, first-pass yield).
- Separate explainable edits from black-box hints to keep auditors calm.
Natural Language Processing for Documentation
NLP turns free-text into structured artifacts: medical-necessity summaries, prior-auth packets, and diagnosis capture from encounter notes. The win isn’t “auto-coding everything”; it’s fewer missing justifications and faster attachments.
- Normalize to vocabularies (CPT/HCPCS, ICD-10, SNOMED CT).
- Keep a reviewer queue for low-confidence spans with inline highlights.
Optical Character Recognition for Paper Claims
Paper isn’t dead—lockboxes and mailed EOBs still happen. OCR + validation pipelines extract line items, map to EDI, and de-duplicate against what’s already in flight.
- Require template/version control, confidence thresholds, and checksum rules.
- Route uncertain fields to a verification worklist; never bury low-confidence PHI in logs.
Medical Billing Automation by Practice Type
Same engine, different tracks. The priorities—and the lift—change with your setting. Here’s how to tune automation without rehashing generic features.
Hospital Billing Automation Solutions
At scale, leakage hides in handoffs. Automate charge capture across service lines, DRG/APC grouping, and prior-auth orchestration so departments stop playing telephone. Route denials by originating unit with playbooks that feed back into coding rules.
-
Department-aware edits and dashboards (surgery vs. radiology vs. ED)
-
Late-charge prevention and CDM governance hooks
-
Worklists that prioritize recoverable dollars, not ticket count
Ambulatory Practice Automation
Ambulatory revenue is won in the minutes around the visit. Same-day edits and real-time estimates keep claims clean before a patient leaves, while point-of-service prompts make copays and coinsurance routine rather than a phone-tag marathon.
Scheduling quietly preps the case—auth packets, missing demographics, plan changes—so front-desk staff aren’t firefighting at check-in. Work queues stay deliberately small and role-aware, the kind a two-person team can clear without overtime or heroics.
Specialty Clinic Billing Systems
Specialties live on nuance: complex modifiers, medical-necessity narratives, biologics/implant tracking, global periods. Build payer-specific playbooks and template-driven documentation so “edge cases” become standard flow.
-
-
Prior-auth kits auto-assembled from specialty templates
-
Inventory/lot capture tied to claims lines
-
-
Modifier validation tuned to NCCI/MUE reality
Telehealth Billing Automation
Virtual encounters add paperwork without the paper. Consent, place-of-service, and time-based coding artifacts are captured as part of the call flow, not as an afterthought. Documentation and supporting images attach asynchronously in the background, preserving the clinician’s cadence while assembling a claim that survives payer scrutiny.
Behind the scenes, scheduling and video events provide the facts—who, where, how long—so the system applies the right POS and modifiers without a scavenger hunt.
Ready-Made vs. Custom Medical Billing Automation Solutions
As with any software, there’s always an option to build a custom coding and billing solution or choose an off-the-shelf product. What are the upsides and downsides of each option?
Off-the-Shelf Solution
The biggest issue with ready-made software solutions is they pack too many features you probably won’t need. That’s because they are trying to serve both enterprises and small to medium-sized businesses. For you, that means overpaying for bells and whistles.
Apart from spending time on finding a perfect solution that has everything you need (and not much beyond), consider:
- Will this billing software integrate with the systems, e.g., EHR, that I already use?
- Do I have any power to introduce any changes to the software in the future?
- Won’t its cost overrun an option of having custom-developed, fully owned software in the long run?
Related: Creating a Hospital Management System
Custom-Developed Billing System
A custom solution will always have the exact features you need and integrate well with your existing infrastructure. In addition, you can add more options as you see fit later on.
On the other hand, developing a custom solution may require a more substantial upfront investment than a ready-made billing platform. At the same time, you can always turn your software into a SaaS solution and get an additional revenue stream for your practice.
Dive deeper into health insurance verification automation to understand how it complements custom billing systems.
Choosing the Right Automation Partner
You’re not hiring coders; you’re buying outcomes. Vet domain depth (payer policy fluency, denial-reduction playbooks), data-custody posture (BAA, PHI pipelines, SBOMs), and roadmap control. Ask for measurable lifts from prior engagements and speak to their ops lead, not just sales. Prioritize:
- HIPAA
- SOC 2
- secure-by-default
Shortlist only HIPAA-compliant automation experts that can show weekly delivery cadence, rollback lanes, and owner visibility into KPIs—not just demos.
5 Steps of Medical Billing Automation
In terms of the development process, creating an automated medical billing system resembles the steps you take to make a medical app. One exception is if you’d like to use AI/ML features, you need one extra stage to create a functional proof of concept.
Here’s a quick rundown on all the required steps for medical billing automation.
| 5 Steps of Medical Billing Automation | |
|---|---|
| Step | Description |
| 1. Discovery | Define ROI goals, tech stack, and essential features in a lean canvas business plan. |
| 2. Functional Proof of Concept | Create a PoC to validate AI/ML algorithms for improved billing and coding efficiency. |
| 3. Rapid Prototyping | Build an interactive prototype and validate UX/UI with user feedback. |
| 4. Development and QA | Iteratively develop features, test functionality, and ensure a smooth deployment. |
| 5. Deployment and Maintenance | Move to production, monitor performance, and plan future updates with tracking tools. |
Step 1: Discovery
The initial phase implies creating a lean canvas with the business plan, including ROI goals, tech stack options, and a list of must-have features. Use Discovery for planning—owners, milestones, payer priorities, and compliance gates—so the rest of the build isn’t guesswork.
Step 2: Functional Proof of Concept
To take advantage of machine learning algorithms to streamline your billing and medical coding processes and improve their accuracy, you must build a quick PoC. This step validates smart algos to see if they help you achieve the required efficiency.
NB: partnering with a healthcare app development company well versed in AI/ML is critical at this stage.
Step 3: Rapid Prototyping
The next move is to prepare an interactive prototype and validate it with end-users, ensuring their feedback is accounted for in the platform’s UX and UI.
Step 4: Development and QA
During the development phase, you will start pushing out biweekly releases, testing the implemented functionality of your medical billing software. Your goal is to proceed with quick iterations, attacking one feature at a time so that you can deploy the solution faster.
Read more on medical billing software development.
Make this disciplined execution: ship short, testable increments with acceptance criteria and demoable outcomes each sprint.
Step 5: Deployment and Maintenance
When all necessary features have been deployed, it’s time to move the platform to a production environment. Post-go-live, schedule enablement to train staff (billers, front desk, coders) on the new workflows and update runbooks.
From this point on, you’ll monitor its performance and user engagement and plan future iterations with the help of automatic tracking tools.
Change Management Strategies
Automation fails when people feel ambushed. Run a super-user model, publish role-based playbooks, and stage rollouts by service line with parallel run and a clear cutover date. Daily war-room the first week; then taper to weekly ops reviews. Incentivize adoption with time-saved dashboards and retired workarounds. A seasoned revenue cycle automation company will also train managers to coach to metrics, not anecdotes—so the new way sticks after go-live.
Measuring Automation Success
Baseline before kickoff, then lock a scorecard:
- clean-claim rate
- first-pass yield
- denial mix by payer/reason
- days in A/R
- cost per claim
- coder minutes per chart
Attribute wins by cohort (location/specialty/payer) to avoid confounding. For AI medical billing solutions, track model drift and false-positive/negative rates alongside dollars. Tie each metric to an owner and an action cadence; if a KPI has no lever, it’s a vanity graph.
Challenges of Medical Billing Automation
“Fully Automated Medical Billing?” Reality check: automation does the heavy lifting, but humans still own edge cases, compliance judgment calls, and payer politics.
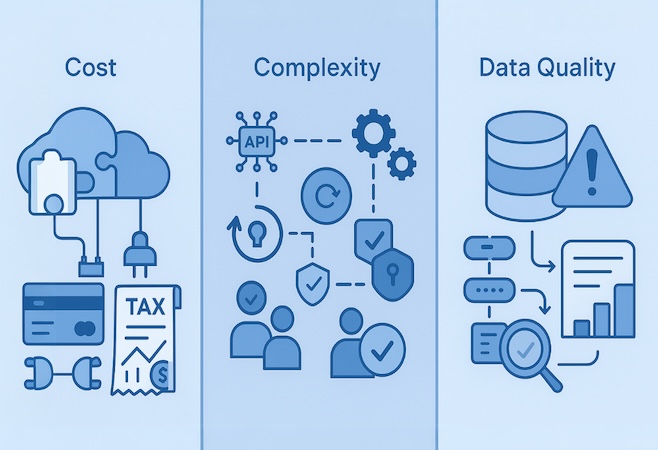
Cost
The price tag isn’t just software. Budget for integrations (EHR/PMS, clearinghouse), rule packs, data cleanup, and change management—plus the drag of staff time during go-live. Hidden costs show up as avoidable denials when you underinvest in eligibility edits, coding validation, or ERA auto-posting. Mitigate with a narrow pilot, reusable components, and a hard ROI lens (first-pass yield, days in A/R, cost per claim).
Complexity
You’re orchestrating multiple moving parts:
- Interfaces: 270/271 eligibility, 837 claim submission, 276/277 status, 835 remits—each with payer-specific quirks.
- Reliability: retries, idempotency, backoff—treat it like a distributed system, not a form launcher.
- Governance: roles/permissions, audit trails, queue-based workflows, and payer-by-payer playbooks.
Data Quality
Garbage in, denials out. Registration errors, mismatched NPIs/Tax IDs, missing prior auths, and inconsistent coding torpedo “clean” claims. Fix upstream: normalize patient/plan data at intake, validate codes and modifiers before submission, and feed denial reasons back into pre-submission rules.
Monitor continuously—data lineage and exception dashboards prevent slow leaks from becoming A/R floods.
Overcoming Billing Automation Challenges
Automation pain points are solvable—if you treat them as design problems, not afterthoughts. Our team of healthcare and technology experts translates operational friction into repeatable patterns you can scale without drama.
Legacy System Integration — Topflight’s Approach
We don’t “wire everything to everything.” We stand up a mediated integration layer with a canonical data model, stable adapters to EHR/PMS/clearinghouses, and contract tests that guard against vendor drift. Golden patient/payer identity prevents duplicate records; replay-safe queues and feature-flagged rollouts de-risk go-lives. Synthetic test beds mirror real payer/EHR edge cases, so the first time you see an exception isn’t after it hits A/R.
Staff Resistance — Our Change Management Support
People don’t resist automation; they resist surprises. We run a super-user model, role-mapped playbooks, and staged cutovers with a parallel run window. Desk-level checklists replace tribal knowledge, and daily stand-ups in Week 1 taper to weekly ops reviews once baseline metrics stabilize. Adoption is reinforced by dashboards that show time saved and rework retired—so the new way becomes the easy way, not another screen to ignore.
Compliance Concerns — Built-in HIPAA Safeguards
Compliance isn’t paperwork; it’s architecture. We build least-privilege access, field-level encryption, immutable audit trails, and data-handling policies into the pipeline from Sprint 1. When appropriate, we leverage Specode’s reusable HIPAA-compliant components (e.g. auth, logging, PHI-safe storage) to accelerate controls without reinventing them. BAAs, SBOMs, and evidence packs are produced as part of normal delivery, so auditors review artifacts you already rely on—no scramble at the end.
Cost Justification — ROI Modeling Services
Budgets move when evidence does. We baseline clean-claim rate, first-pass yield, denial mix, coder minutes per chart, and days in A/R, then model scenarios (by payer, specialty, site) to forecast lift. Pilots get stage-gates with hard success criteria and a roll-forward plan only if the math clears. The output is a board-ready case: expected recovery dollars, payback period, sensitivity bands, and what to cut next if results stall.
Topflight’s Medical Billing Technology Stack
We don’t chase shiny tools; we assemble a stack that moves claims from “pending” to “paid.” Topflight’s proven methodology for billing automation aligns architecture to payer reality, EHR constraints, and evidence requirements—so you scale accuracy, not headaches.
AI and ML Capabilities
NLP for code suggestion, ML risk scoring for pre-submission edits, and anomaly detection by payer/specialty. Models ship in shadow mode first, then behind acceptance thresholds with human-in-the-loop.
- Hybrid rules + ML to keep decisions explainable.
- MLOps: model cards, replay tests, drift monitors, rollback lanes.
Cloud Infrastructure Options
AWS, GCP, or Azure using HIPAA-eligible services, containerized workloads (Kubernetes) for core apps, and serverless bursts for OCR/ETL.
- Single-tenant or VPC-peered footprints; data-residency controls.
- Managed Postgres + event queues for durable, idempotent workflows.
Security and Compliance Features
Least-privilege IAM, field-level encryption (KMS/HSM), immutable audit logs, and secrets vaults baked in from Sprint 1. When speed matters, we lean on Specode’s reusable HIPAA-compliant components (auth, logging, PHI-safe storage) to accelerate without cutting corners.
- SBOM + SAST/DAST in CI; change-controlled releases with evidence packs.
Integration Capabilities
A mediated adapter layer speaks FHIR R4/HL7 v2 for clinical data and X12 (270/271, 276/277, 837, 835) for revenue cycle, with contract tests guarding against upstream drift.
- Case-by-case EHR and clearinghouse integrations via native APIs or middleware (e.g., Mirth), replay-safe queues, and versioned schemas to keep cutovers calm.
Building Custom Medical Billing Automation with Topflight
How topflight transforms medical-billing automation ideas into investor-grade products — that’s the bar we optimize for.
Medical-billing automation lives or dies on airtight code accuracy and denial-proof workflows—not on who can shout “AI” loudest at a trade show.
Our Healthcare Automation Expertise
That’s why founders behind GaleAI tapped Topflight to turn a proof-of-concept into a market-ready platform. In just 1,100 engineering hours we delivered an MVP that now identifies CPT codes in seconds, lifts provider revenue up to 15 %, and slashes coding effort 97 %—while surfacing 7.9 % more billable codes than human reviewers. Those wins aren’t a one-off.
-
AI-first RCM accuracy – NLP and deep-learning models surface every payable CPT/HCPCS code, stamping out under-coding before it hits the payer.
Topflight’s broader playbook—AI consulting, secure health-data integration, and revenue-cycle automation—anchors the “Why healthcare leaders trust us” section on our own homepage . And the results travel: clients we’ve engineered products for have raised more than $188 million in follow-on funding to date.
Custom vs Off-the-Shelf Solutions
Off-the-shelf gets you speed; ownership gets you leverage. As custom billing system developers, we prioritize evidence over demos—instrumenting lift (clean-claim rate, first-pass yield) at MVP so you can scale what works and kill what doesn’t.
-
Investor-ready dashboards – Recovery rates, denial velocity, and revenue lift instrumented at MVP stage, arming you with metrics VCs underwrite.
Integration with Major EHR Systems
Great automation dies at brittle seams. We design for real-time checks and clean hand-offs across EHR/PMS/clearinghouses so operations don’t stall.
-
Real-time payer connectivity – Eligibility, benefits, and prior-auth APIs resolve in seconds, turning “call the payer” hold music into a relic.
Compliance-First Development Approach
As healthcare technology specialists, Topflight understands that auditors fund evidence, not promises—so compliance is built in from sprint one, not papered over at the end.
-
Compliance baked in – HIPAA, SOC 2, and PHI-safe cloud pipelines from sprint one keep auditors yawning, not gasping.
Cost of Automating Medical Billing
The cost of automation in medical billing will depend on the scope of your solution. If you envision AI/ML as the core part of the software, the price will probably be between $150,000 and $200,000. And if you’re looking to automate medical billing without reverting to AI algorithms, you need to budget around $80,000 — $120,000. Minimal viable product for both scenarios.
I also encourage you to read about the cost to develop a health insurance app in our dedicated blog.
If you want to automate medical billing at your practice by creating a custom web or mobile solution, get in touch with our experts. We’ll be happy to share our expertise.
[This blog was originally published in June 2022 and has been updated for more relevant content]
AI/ML capabilities to parse speech, text, and images. If you want to start small and get immediate benefits, build a custom solution. No. You’re absolutely free to pick any technology. In fact, your choice should be based on how well this or that tech stack allows for integrating with your existing systems. Between $80,000 and $200,000, depending on the scope. Map your workflow, then automate the high-yield steps first: eligibility checks, ML-assisted code validation, clean electronic claims, and ERA auto-posting; keep humans on exceptions, pilot one service line, and track first-pass yield and days in A/R.Frequently Asked Questions
What are the top trending features in medical coding solutions?
Should I build a custom medical billing solution or get a SaaS subscription instead?
Is there a tech stack recommended for creating an automated billing solution?
How much does it cost to build an automated healthcare billing system?
How do I automate medical billing and coding?