Just like a masterful conductor orchestrates a symphony, medical device integration harmonizes the flow of patient data in the healthcare sector. It’s the invisible maestro, ensuring each instrument (or, in our case, device) plays its part flawlessly, contributing to a melodious performance – improved patient care. So, let’s delve into this fascinating world of medical hardware integration, where technology and healthcare join hands to compose a healthier future.
Top Takeaways:
- Medical device software integration is revolutionizing healthcare. It’s like a skilled conductor, bringing diverse medical devices together, enabling them to ‘play’ in sync, and creating a seamless flow of data that enhances patient care.
- Through medical device data integration, we are transitioning from disjointed solos to a well-coordinated orchestra. This approach automates the capture and analysis of valuable patient data, eliminating manual errors and saving precious time for clinicians.
- Interoperability is the sheet music guiding this orchestra. It’s the key to successful performance, facilitating the seamless exchange of data among various systems, devices, or applications, thereby enhancing the overall quality of care.
Table of Contents:
-
- Understanding Medical Device Integration
- Key Components of Medical Device Integration Software
- Benefits and Challenges of Medical Device Integration Software
- Examples of Successful Integration of Medical Devices
- Medical Device Software Integration: Ways of Implementation
- Why Topflight Is the Go-To Partner for Device-to-EHR Integration
- Medical Device Software Integration Best Practices
Understanding Medical Device Integration
What is medical device integration? Medical device integration (MDI) is a revolutionary approach in the healthcare industry, enhancing patient care and streamlining clinical workflows. Essentially, it involves the seamless flow of data from medical devices to a hospital’s or clinic’s information system.
Modern healthcare requires seamless handling of medical data and health information, making MDI crucial for maintaining accurate and accessible health records across various departments.
But what exactly does it entail, and why is it becoming increasingly vital in today’s digital healthcare landscape?
- Data Collection and Analysis: At the heart of medical device integration lies the concept of efficient data collection. Medical devices generate a wealth of valuable patient data. However, without proper integration, this data can remain untapped. MDI enables the automatic capture and analysis of this data, eliminating manual input errors and saving clinicians’ time.
Connected medical devices generate continuous streams of vital patient information, while administrative processes ensure this data is properly logged and managed within the healthcare IT infrastructure.
- Interoperability: One of the primary goals of MDI is to facilitate interoperability – the ability of different systems, devices, or applications to connect and exchange data in a coordinated manner. This interoperability allows for a more cohesive, unified patient care approach.
- Patient-Centric Care: By integrating medical devices, healthcare providers can access real-time patient data, thus enabling immediate response to any changes in the patient’s condition. This capability is not only beneficial for patient outcomes but also enhances the overall patient experience.
- Cost Savings: While the initial investment may seem substantial, the long-term cost savings associated with MDI are significant. Streamlined workflows, reduced manual labor, decreased errors, and improved patient outcomes all contribute to financial efficiency.
Also Read: EHR Interoperability Guide
According to a study by the West Health Institute, medical device integration could save the U.S. health system an astounding $30 billion per year by increasing productivity and efficiency.
Here are a few eye-opening statistics that underscore the significance of medical sensor integration and its potential impact on the healthcare system:
- As per the FDA’s annual report in 2022, there were nearly 6,000 medical device authorizations.
- The Center for Devices and Radiological Health at the FDA granted marketing approval to 124 innovative devices in 2023, marking the highest number in the Center’s archives.
- As per KPMG, the medical device sector is seeing consistent expansion, with projected annual global sales growth of more than 5%, aiming to hit close to US$800 billion by 2030.
The path to market for integrated medical solutions often involves rigorous medical device clinical trials to ensure safety and efficacy. These trials are especially critical when integration involves multiple devices or novel data collection methods.
The future of healthcare lies in its ability to adapt and innovate. As we move towards a more connected world, the importance of medical device integration becomes increasingly evident. It’s no longer just a luxury; it’s a necessity. The question is, how can healthcare organizations successfully leverage this powerful tool?
In the next section, we’ll delve into the key components of medical device integration software.
Key Components of Medical Device Integration Software
In the world of healthcare, medical device integration software has become a critical cog in the machinery. As we’ve established, it not only enhances patient care but also streamlines clinical workflows, making it an indispensable tool for healthcare providers. But what precisely are the key components that make up this essential system?
1. Device Connectivity
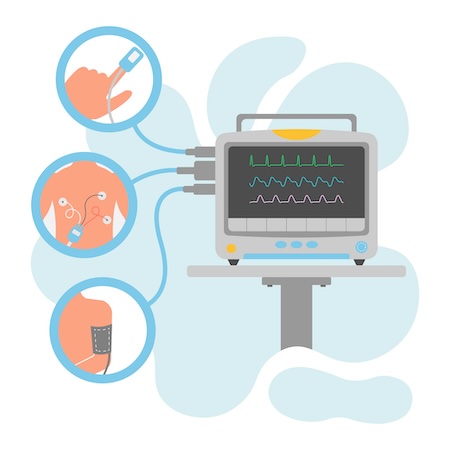
One of the core components of medical device integration software is the ability to connect and communicate with various medical devices. This includes everything from ventilators to heart monitors. The software must be able to receive data from these devices and transmit it to the necessary platforms for analysis and access by clinicians.
2. Data Normalization
Data normalization is the process of transforming raw data from medical devices into a standardized format. This is crucial because different devices may produce data in different formats. Normalization ensures that all the data can be understood and interpreted consistently, regardless of its source.
3. Data Security
As with any system dealing with sensitive patient information, data security is a vital component of medical device integration software. This includes features like encryption, access controls, and audit trails to prevent unauthorized access and protect patient confidentiality.
4. Interoperability
Interoperability refers to the ability of the software to work seamlessly with other systems, such as EHR systems. This means that the data collected from medical devices can be easily integrated into a patient’s EHR/EMR, providing a comprehensive view of the patient’s health.
Configuration and compatibility features ensure devices can work together seamlessly, while verification processes maintain data accuracy and system reliability.
Check out our EHR integration services
5. User Interface
Finally, the user interface is a critical component of medical hardware integration software. It needs to be intuitive and user-friendly, enabling clinicians to easily view and interpret the data from the connected devices. A well-designed user interface can significantly improve workflows and enhance patient care.
These elements work together to provide an efficient and effective solution for integrating medical devices into healthcare workflows. And remember, while these components are critical, they’re just the tip of the iceberg.
There are many other factors to consider when implementing medical device integration, such as ensuring compliance with regulatory standards and selecting suitable medical device systems integrators. But don’t worry – we’ll delve into these topics and more in the sections to follow. So, are you ready to take the next step in your journey towards successful medical sensor integration?
Benefits and Challenges of Medical Device Integration Software
Just like any other technological evolution, the process of medical device software integration is not without its ups and downs. While it brings along a sea of benefits that can revolutionize healthcare provision, there are also challenges that need to be navigated carefully. Here, we explore both sides of the coin.
Benefits of Medical Device Integration Software
The integration of medical devices into healthcare workflows can significantly enhance patient care and improve operational efficiency. Let’s delve into some of the key benefits:
- Improved Patient Care: The use of medical hardware integration software allows for real-time monitoring of patients’ health data. This facilitates timely interventions by clinicians and enables personalized care, leading to better health outcomes.
- Enhanced Efficiency: Automating data collection and integration eliminates the need for manual data entry, reducing the risk of errors and freeing up valuable time for healthcare providers to focus on direct patient care.
- Comprehensive Access to Patient Information: When medical devices are integrated with EHR systems, clinicians gain a holistic view of a patient’s health data. This comprehensive information supports informed decision-making and ultimately leads to improved patient outcomes.
- Remote Monitoring Capabilities: For patients with chronic conditions or those requiring continuous monitoring, medical device integration software offers the benefit of remote monitoring. Clinicians can keep a watch on patients’ health status from afar, ensuring timely intervention when necessary. This capability extends to various monitoring devices like fall detectors, infusion pumps, and other specialized equipment, enabling both caregivers and therapists to provide comprehensive care.
- Data-driven Insights: By coupling medical device data with analytics tools, healthcare organizations can glean valuable insights about patient populations, treatment effectiveness, and overall healthcare trends. These insights can drive evidence-based decision-making and improvements in care delivery.
Furthermore, advances in computer vision in healthcare are enhancing these capabilities, enabling AI-powered analysis of medical imaging data and automated patient monitoring systems.
The Beauty of RPM Services with MDI Software
The integration of telehealth functionality allows healthcare providers to extend their reach beyond traditional care settings, making healthcare more accessible and convenient for patients.
One trend that’s particularly exciting in the realm of medical device integration is the burgeoning ability to offer personalized Remote Patient Monitoring (RPM) services on a subscription basis. But why is this so revolutionary?
Related: Remote Patient Monitoring App Development Guide
Well, it essentially means that healthcare providers can tailor their monitoring services to each patient’s specific needs, thus enhancing the precision and effectiveness of care. Imagine having a healthcare plan that adapts to you rather than just fitting into a one-size-fits-all box. This development is not just about convenience; it represents a fundamental shift towards more patient-centric healthcare.
- Customized Care Plans: With personalized RPM services, patients receive care that’s specifically tailored to their health conditions and requirements.
- Access to Healthcare: It also breaks down barriers to access, making it easier for patients in remote or underserved areas to receive high-quality healthcare services.
- Cost Efficiency: Subscription-based models can often be more cost-effective for patients, especially those with chronic conditions who require continuous monitoring.
- Empowered Patients: By providing patients with more personalized and accessible care options, RPM services empower them to take an active role in managing their health.
The beauty of personalized RPM services lies in their ability to transform healthcare into a more attentive, responsive, and patient-focused service. With medical hardware integration paving the way, the future of healthcare looks not only more competent but more compassionate and personalized than ever before.
Check out our healthcare app development services
Challenges of Medical Device Integration Software
Despite the numerous benefits, the path to successful medical device integration is littered with obstacles. Here are some of the key challenges:
- Interoperability Issues: Medical devices often use different data formats and communication protocols, creating hurdles in seamless integration. Ensuring interoperability between various devices and systems requires careful planning and coordination.
- Data Security and Privacy Concerns: With integration comes the risk of data breaches. Healthcare organizations need to implement robust security measures to protect sensitive patient information and comply with data protection regulations.
- Complex Implementation Process: The implementation of medical device data integration software can be a long and winding road, requiring collaboration between healthcare providers, IT teams, and device manufacturers (those firmware updates can be painful to integrate sometimes!).
- Adapting to Evolving Regulatory Requirements: The dynamic nature of regulations in the healthcare sector means manufacturers must stay updated with the latest regulatory changes. This can be incredibly challenging for small to medium-sized companies without a dedicated regulatory staff, especially when medical integration touches anywhere near software as a medical device certification or AI/ML.
- Cost Considerations: Developing and implementing healthcare device integration software involves significant upfront costs. Careful evaluation of the return on investment and long-term cost implications is crucial for healthcare organizations.
- Training and User Adoption: New technology invariably requires training and change management efforts. Ensuring user adoption and proficiency with the medical device integration software is critical to maximizing its benefits.
As you can see, while medical device integration software offers numerous advantages, such as improved patient care, enhanced efficiency, and insightful data analysis, it also presents challenges that must be navigated carefully. This is particularly true for software-based medical devices, where SAMD clinical evaluation has become a cornerstone of regulatory compliance and quality assurance. Overcoming these issues requires strategic planning, collaboration, and investment in the right technology solutions.
At Topflight, we understand these challenges and have the expertise to guide your organization through the process of IoT healthcare development. Our team of experts can help you navigate the complexities of medical sensor integration, ensuring a smooth and successful implementation that meets your organization’s unique needs.
Stay tuned for examples of successful integration of medical devices in the next section and ways to implement medical device software integration.
Examples of Successful Integration of Medical Devices
As we delve deeper into the realm of medical device integration connecting healthcare solutions with hardware sensors, real-world examples can provide invaluable insights into how this technology can revolutionize healthcare provision. Let’s examine three instances where medical hardware integration has been successfully implemented, resulting in improved patient care and streamlined workflows.
Also Read: Healthcare App Development Guide and Medical Device Software Development
Dedica Health: Remote Patient Monitoring Platform
One standout example is Dedica, a company that leveraged a remote patient monitoring platform to upgrade its care delivery model while adhering to Medicare guidelines. This platform replaced error-prone systems like spreadsheets with a comprehensive solution that helped follow Medicare RPM/CPT requirements, reduce the volume of phone calls, and eliminate manual tasks.
Key achievements of the platform include:
- Monitoring over 1,100 patients daily
- Securing a $300,000 ARR deal for RPM via a SaaS subscription
- Achieving CPT code targets for more than 80% of patients
The platform was developed with a focus on the following features:
- Integration with clinically certified medical sensors
- Automated back-office routines
- Health data visualization
- Compliance with HIPAA regulations and audit trail
RTHM: Real-Time Health Monitoring Platform
RTHM leads in pioneering research, diagnostics, and remote care for individuals with Long COVID, ME/CFS, and other co-occurring conditions. Recognizing the escalating expenses tied to treating these conditions, RTHM decided to establish a digital ecosystem that connects patients, providers, and researchers.
The highlights of their journey include:
- Developing a solid MVP to gain traction with patients
- Using a no-code/low-code infrastructure for fast pivoting
- Ensuring strong security in line with HIPAA guidelines
The platform they built includes a mobile app for patients and an admin area for RTHM staff. The patient app allows individuals to monitor their conditions, track symptoms, and follow treatment plans, while the admin area enables physicians to diagnose and recommend treatment based on patients’ PHI.
IoMT: Integrated Skin Scanning Med Sensor
Another successful example of medical device integration comes from a venture-funded RPM company. They built a proprietary electron spectroscopy device and partnered with us to develop a host of software solutions for clinics to administer the device.
Since our partnership in 2017, we have deployed UI/UX, full-stack development, QA, and HIPAA compliance to support their vision. The partnership has helped the company raise $34 million.
These examples highlight the transformative impact of medical sensor integration on healthcare delivery. They underscore how integrating devices with software platforms can streamline workflows, enhance patient care, and drive growth for healthcare organizations.
It’s also worth noting that the integration of wearable technology in healthcare is a growing trend that offers exciting opportunities for data collection and patient monitoring. As shown in these examples, the potential for innovation in this field is vast, and the rewards are significant.
In the next section, we’ll explore various ways to implement medical device software integration, providing practical advice to help you navigate this complex process.
Medical Device Software Integration: Ways of Implementation
In the rapidly advancing world of healthcare technology, MID is no longer a luxury but a necessity. However, implementing it can be a complex process, requiring careful planning and execution. In this section, we’ll explore various ways to successfully implement medical device software integration.
Major Considerations for Medical Device Integration Projects
Embarking on a medical device data integration project is not a decision to be taken lightly. It comes with its unique set of considerations and prerequisites. Here are some crucial points you should bear in mind:
- Existing Health App: Before you begin, it’s essential to have an existing health app or system, or at least a concrete plan to build one. This will serve as the foundation for your medical device integration.
- Device Selection: Choosing the right medical device is critical. Once you’ve made a choice, you’ll be essentially locked into its capabilities, such as supported data types, encryption standards, and more.
- Destination System: Typically, the destination for integrating a medical device will be an EHR system. Therefore, understanding the intricacies of EHR systems is paramount.
- Part of a Larger Project: Remember, health device integration is just a part of a larger healthcare software development project. While certain steps like prototyping may not be essential, others like discovery and automated testing are vital.
- Discovery Phase: The discovery phase is essential as it allows you to draft an architecture, define the feature set, and align expected KPIs with your ROI targets. At this stage, you’ll also need to choose a medical device, effectively locking yourself into a specific feature roadmap.
- Automated Testing: With the vast amount of data exchanged between medical sensors and software, automated testing is a must. It’s virtually impossible to manually verify data mapping and its comprehensiveness.
- Hardware and API Versioning: Your software should be able to identify hardware versions and work with API versioning. This becomes particularly important if you plan to update your hardware with firmware upgrades or expand to other devices in the future.
- MVP Development: Instead of a full-fledged version, focus on developing a Minimum Viable Product (MVP) for your app. This will allow you to launch, sign up patients, measure KPIs, and make improvements based on real-world feedback.
By keeping these considerations in mind, you can ensure a smoother implementation process for your medical device integration project. Let’s cover the rest of the major points you’ll need to address when implementing medical device software integration.
Vendor Selection: Aligning with the Right Partners
Choosing the right medical device integration vendors is a critical first step. Look for vendors with a proven track record in the healthcare industry, experience in implementing similar projects, and the ability to provide post-implementation support. Here are some considerations:
- Expertise: The vendor should have a deep understanding of healthcare regulations, data privacy standards, and the specific requirements of medical sensor integration.
- Scalability: As your needs evolve, the vendor should be able to scale their medical device integration services to match your growth.
- Support: Post-implementation support is crucial. The vendor should provide timely assistance to address any issues that may arise after the integration is complete.
Interoperability: Ensuring Seamless Data Flow
Interoperability refers to the ability of different systems and devices to exchange and interpret shared data. In the context of medical sensor integration, it involves ensuring that your integrated devices can seamlessly communicate with each other and your existing IT infrastructure. Key aspects include:
- Standardization: Adopting standardized data formats and communication protocols, such as HL7, FHIR, and DICOM, can facilitate interoperability.
- Data Integrity: Proper data validation processes should be implemented to maintain the integrity of the data exchanged between devices.
- Data mapping: Mapping data fields between readings generated by medical sensors and EHRs or other healthcare systems is crucial for successful interoperability.
- Testing: Rigorous testing should be conducted to verify that all integrated devices can effectively exchange and interpret data.
For those intrigued by the potential of FHIR in modern healthcare solutions, our dedicated article on FHIR app development offers a comprehensive overview, from concept to deployment, equipping you with the knowledge to innovate confidently.
Security and Compliance: Safeguarding Patient Data
In healthcare, data security and regulatory compliance are paramount. When integrating medical devices, these aspects must be meticulously addressed. Here’s what you should focus on:
- Data Encryption: All data transmitted between devices should be encrypted to protect against unauthorized access.
- Access Rights: Implement strict access rights controls to ensure that only authorized personnel can access sensitive patient data.
- Regulatory Compliance: Ensure your integration adheres to all relevant regulations, including HIPAA and GDPR.
Related: HIPAA Compliant App Development Guide
Analytics: Leveraging Data for Insightful Decisions
Medical device integration generates a wealth of data that can provide valuable insights for healthcare providers. Implementing robust analytics capabilities can help you make the most of this data. Key steps include:
- Data Aggregation: Collect and consolidate data from various devices into a centralized database.
- Data Analysis: Use advanced analytics tools (using AI/ML) to analyze the aggregated data and extract meaningful insights.
- Reporting: Generate comprehensive reports to inform decision-making and improve patient care.
Continuous Improvement: Learning from Feedback
Finally, it’s important to remember that medical device integration is not a one-time project but an ongoing process. Regularly review your integration’s performance, gather feedback from end-users, and make necessary adjustments to continually improve its effectiveness and efficiency.
Implementing medical device software integration can be a complex process, but with the right approach and resources, it can yield significant benefits. By choosing the right vendors, ensuring interoperability, safeguarding data security, leveraging analytics, and continuously improving, you can successfully integrate medical devices and transform your healthcare delivery.
Read more on medical device cost breakdown
Why Topflight Is the Go-To Partner for Device-to-EHR Integration
Topflight’s edge-to-cloud playbook turns raw sensor output into clinician-ready insights—without blowing timelines or budgets:
-
Joovv light-therapy IoT refresh – We replaced USB data dumps with BLE commands, React Native apps, and HIPAA-tight syncing to Apple HealthKit and Google Fit.
-
Dedica cardiac-RPM rollout – Our real-time vitals pipeline now serves 1.1 k+ patients, helps 80 % hit Medicare CPT targets, and kicked off a six-figure ARR SaaS deal straight from the MVP.
Why teams choose Topflight
-
Device & EHR fluency – BLE, Wi-Fi, MQTT, SMART-on-FHIR, HL7 v2… we already speak the protocols your hardware and hospital use.
-
Cross-platform velocity – One React / React Native codebase covers iOS, Android, and web, trimming 40-50 % off dev hours.
-
Compliance baked in – HIPAA, IEC 62304, SOC 2, and audit trails ship from sprint one, so security reviews don’t stall launches.
-
Dashboards that speak CFO & clinician – Sub-second alerts, reimbursement metrics, and usage analytics wired in at MVP.
Medical Device Software Integration Best Practices
Medical sensor integration is a sophisticated process, and I’ve seen firsthand how following best practices can streamline this process and lead to successful outcomes. Let’s delve into these best practices that have provided medical device integration success for many organizations.
Understand Your Data
Before you start integrating, you need to understand your data thoroughly. This involves knowing the type of data you’ll be dealing with, its sources, and how it will be used. Key steps include:
- Identify the various data elements that the medical device will capture.
- Understand the data format and how it will be translated into a format that your healthcare system can interpret.
- Evaluate how the data will be used by doctors and other healthcare professionals.
Understanding your data will help you make informed decisions about integration and ensure that the data serves its intended purpose effectively.
Implement a Data Sync Engine
One of the best practices in medical device software integration is implementing a data sync engine. This acts as a hub between the medical device and the healthcare system it integrates with, such as an EHR system. Here’s why this is beneficial:
- All data from sensors comes to a unified repository, gets normalized, and is only then shared with other systems.
- It simplifies data management and ensures consistency across platforms.
- Integrating with new solutions becomes easier and faster.
By acting as a bridge between your medical device and the healthcare system, a data sync engine (like Mirth) can significantly enhance the efficiency and effectiveness of your integrations.
Read more on Mirth integration
Leverage Cloud-Native Architecture and APIs
Cloud-native architecture and APIs are powerful tools for medical device integration. They offer numerous benefits, including scalability, flexibility, and cost-effectiveness. Here’s how they can help:
- Scalability: Cloud-native architecture allows you to scale your integration quickly as your needs grow.
- Flexibility: APIs enable seamless communication between different systems, allowing you to integrate a wide range of medical devices with various healthcare systems.
- Cost-Effectiveness: By leveraging cloud services and APIs, you can reduce the cost of integration and ongoing maintenance.
Invest in Regular Assessments and Training
Regular assessments and training are vital for successful medical device integration. They ensure that your integration continues to meet its objectives and that your team has the skills to manage it effectively. Key aspects include:
- Regular Assessments: Regularly assess the performance of your integration, identify any issues, and make necessary adjustments.
- Training: Train your team on how to manage the integration, interpret the data, and handle any issues that may arise. This is particularly important for biomedical professionals who will work closely with the integrated system.
Plan for Resource Management
Proper resource management is vital for successful medical hardware integration. This involves ensuring that you have the necessary resources to implement and maintain the integration and that these resources are used efficiently. Key steps include:
- Identify the resources you’ll need for the integration, including hardware, software, and personnel.
- Develop a plan to manage these resources efficiently throughout the integration process.
- Regularly review your resource usage and make adjustments as needed to ensure optimal efficiency.
By following these best practices, you can streamline your medical device software integration process and achieve successful outcomes. Remember, successful integration is not just about connecting a medical device to a healthcare system; it’s about ensuring that this connection delivers value to your organization and improves patient care.
In sum, navigating the complexities of medical device integration software need not be a solitary voyage. Allow our seasoned experts to guide your endeavor, transforming challenge into opportunity and complexity into simplicity.
If you’re poised to redefine the future of healthcare with seamless medical device integration, reach out today. Together, we can unlock the full potential of your medical technology.
[This blog was originally published on March 4, 2024, but has been updated for more recent data]
FAQ
How much does medical device integration software development cost?
The cost of medical sensor integration software development can vary greatly depending on several factors, including the complexity of the project, the number of devices to be integrated, the technologies used, and the vendor’s rates. It’s best to consult with a software development company like Topflight to get an accurate estimate based on your specific needs.
What technologies are used to integrate medical devices?
Several technologies can be used for medical device integration. These include standardized data formats and communication protocols like HL7, FHIR, and DICOM, APIs for seamless data exchange, cloud-native architecture for scalability, and data sync engines for efficient data management.
How does the integration of medical equipment affect patient care?
Medical hardware integration can significantly enhance patient care. It allows for real-time data capture from various medical devices, enabling doctors to make informed decisions based on comprehensive, up-to-date patient information. It also improves efficiency, enabling healthcare professionals to spend more time on patient care and less time on manual data entry.
How does the integration of medical equipment affect hospital workflows?
By automating data capture and exchange, medical sensor integration can significantly streamline hospital workflows. It eliminates the need for manual data entry, reducing errors and freeing up staff time. It also ensures that all patient data is readily available in the EHR system, facilitating seamless coordination between different departments.
How can healthcare facilities implement medical device integration?
Implementing medical device integration involves several steps, including understanding your data, choosing the right medical device integration vendors, ensuring interoperability, safeguarding data security, leveraging analytics, and continuously improving based on feedback. It’s advisable to work with an experienced software development company like Topflight to ensure a successful implementation.
What medical devices can be integrated with each other?
Virtually any medical device that captures patient data can be integrated with others. This includes devices like blood pressure monitors, glucose meters, ECG machines, pulse oximeters, and more. The key is to ensure that the devices use compatible data formats and communication protocols and that the medical device data integration adheres to all relevant data privacy and security standards.