Chiropractor app development isn’t about “an app,” it’s about owning the workflow from booking to documentation to payment without creating five new problems in the process. If you’ve felt the swivel-chair pain between scheduling, intake, SOAP notes, and billing, you already know where the ROI hides: fewer no-shows, faster note closure, cleaner claims.
This guide cuts past demo theater and shows what a v1 must prove, how to design PHI boundaries that pass audits, and where a patient app, provider console, and integrations actually pay for themselves.
We’ll also be blunt about build vs. buy, what timelines and budgets look like in the real world, and when AI—posture analysis, ROM from video, RTM—moves clinical decisions rather than just pretty charts. If you want a clinic OS, not another widget, you’re in the right place.
Key Takeaways
- MVP wins by nailing scheduling, intake/consent, payments, and reminders; everything else can wait.
- For chiropractic app development, design compliance as architecture: one auth layer, audit you can query, PCI outside HIPAA.
- AI belongs only where it drives treatment decisions and adherence; measure outcomes, not vibes.
Table of Contents
- Understanding Chiropractor App Development
- Chiropractic App Market Overview
- Types of Chiropractor Apps
- Essential MVP Features for a Custom Chiropractor App
- Advanced Clinical Features for a Chiropractic Mobile App
- Step-by-Step Development to Create a Chiropractor Application
- Technology Stack Recommendations
- Compliance That Ships: HIPAA, PCI and Insurance Verification
- Monetizing Your Chiropractor App
- Challenges and Solutions for Developing a Chiropractor Application
- AI/ML Implementation for Clinical Outcomes
- Build vs. Buy Decision Framework
- Development Cost Breakdown
- North-Star Metrics for Chiro Apps
- How Topflight Can Help You Build an App for a Chiropractor Clinic
Understanding Chiropractor App Development
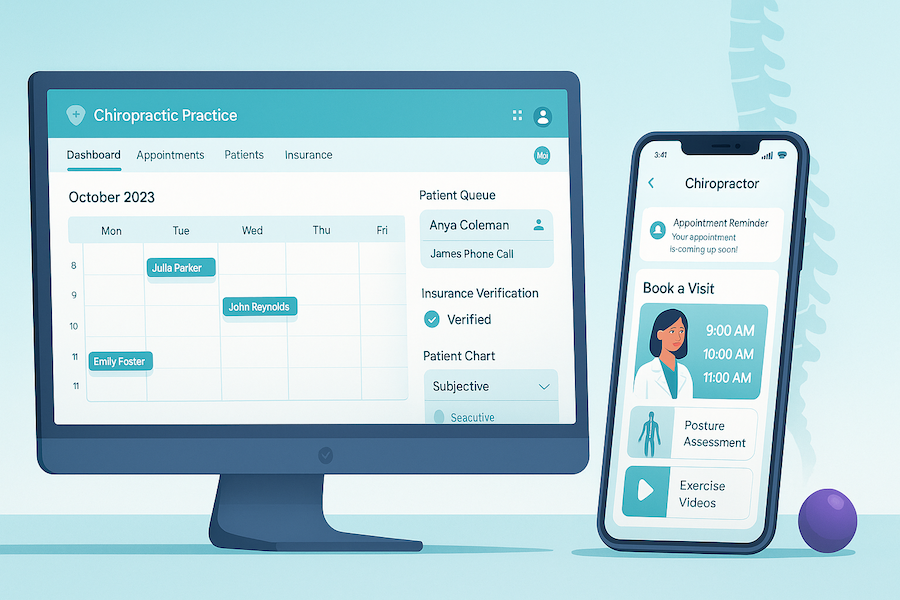
What is chiropractor app development? Chiropractor app development is the process of creating mobile applications that streamline clinic operations, improve patient engagement, and enhance treatment outcomes.
It extends beyond a patient app: most real-world builds pair a patient-facing mobile experience with a provider/staff console for scheduling, SOAP notes, billing, and secure messaging. To avoid swivel-chairing, your app should plug into existing clinic management and patient management systems—often via APIs or HL7/FHIR—and exchange charts with electronic health records (EHRs).
The goal: one clean workflow from booking to documentation to payment—PHI fenced, audit-ready, and measurable.
If you need to build an app for chiropractor workflows fast, start with scheduling, intake/consent, payments, and reminders—prove v1 on those before you add anything cute.
Chiropractic App Market Overview
If you’re building for chiropractic workflows, expect a SaaS-heavy, cloud-tilted market where buyers care about practice analytics and multi-location sanity. Here’s the U.S. snapshot.
Key statistics (US, 2020–2025):
- ~40,000 chiropractic offices form the addressable provider base adopting digital tools.
- Market size: $245M–$1.2B (2024–2025); projected $525M–$2.5B by 2030–2033; CAGR 5.3%–11.3%, depending on segmentation and AI adoption.
- Cloud now ~62% of deployments (vs. ~38% on-prem), driven by lower CapEx, better updates/security, and easier multi-location support.
“Chiropractors treat more than 35 million Americans (adults and children) annually.”
American Chiropractic Association (ACA)
Pricing & Packaging in the Wild
Entry platforms typically start around $199 per provider per month; mid-tier lands in the $299–$399 range, and premium tiers push $500–$600+ once you add deeper practice analytics and integrations.
If you outsource revenue cycle, expect 3–7% of collections plus a fixed $200–$600 monthly base.
“Medicare currently only reimburses for a single chiropractic service: manual manipulation of spine-related conditions.”
American Chiropractic Association (ACA)
Vendor Landscape and Outcomes
Chiro-specific systems (think ChiroTouch, ChiroFusion, SimplePractice, Genesis) win most SMB deals; the massive enterprise EHRs rarely make sense here—cost/complexity tax is real.
- Measured ops lift: reports of ~15% fewer claim denials, 25% faster reimbursements, and 20–30% lower admin overhead after modernizing stack.
- Retention signal: case-level evidence shows up to ~40% patient-retention increase with loyalty/app programs (directionally relevant for outpatient).
Modernizing the stack consistently correlates with fewer claim denials, faster reimbursements, and lower admin overhead; loyalty/app programs can materially lift patient retention.
Types of Chiropractor Apps
Modern stacks fall into five patterns. Pick the one that moves core metrics (no-shows, accounts receivable (AR) days, note closure), not the one with the flashiest demo.
1. Practice Management & EHR (the clinic OS)
A chiropractic practice management app that runs the back office end-to-end: EHR, appointment scheduling, intake, billing/claims, reports, roles, and multi-location as a tier— not a separate product. Usually ships with a basic patient portal for records, forms, and receipts.
Use when: workflow control and integrations matter.
Red flag: no export/APIs → future migration tax.
2. Patient Engagement & Patient Portal (the patient’s app)
A patient-facing chiropractic mobile app + patient portal for self-booking, reminders, payments, secure messages, and prescribed exercise videos.
Job to be done: cut no-shows and activate follow-ups without front-desk heroics.
Musts: consent, retention policy, audit trail.
3. Telehealth & Virtual Care
HIPAA video, triage, screen share, document handoff to the chart.
Use when: access and convenience drive adherence. Non-negotiables: BAA in place, recordings/notes retained per policy.
4. Specialized Clinical & Diagnostic Tools
Posture capture, ROM via sensors, digital goniometers, 3D spine modeling, image annotation.
Reality check: great for objective measures; useless if they don’t push structured results back into the record.
5. Booking-Only Solutions
A lightweight chiropractor booking app focused on discovery, appointment scheduling, reminders, and basic payments.
Good for: quick demand gen and testing offer/price.
Risk: data silos if it can’t sync with your PMS/EHR.
Fast Chooser
- Single site, standard workflows → start with Booking-Only + Patient Portal; upgrade when ops strain.
- Growing clinic, multi-location, insurance → go Practice Management & EHR first; add engagement later.
- Remote/hybrid care model → pair Telehealth with your EHR; don’t let video live off the chart.
Essential MVP Features for a Custom Chiropractor App
When teams create chiropractor application v1, ship the few workflows that move revenue and reduce admin drag—nothing ornamental. A patient-facing layer plus a lean admin console is enough.
- Patient intake forms + consent forms: pre-visit, mobile-first, e-sign, and mapped to chart fields. No PDFs in email. Log every change. If patients Google “patient intake app chiropractor,” this is what they expect to complete in under 5 minutes.
- Scheduling + rescheduling: real-time slots, provider rules, buffers, and waitlists. Cards-on-file at booking to curb no-shows.
- Appointment reminders: SMS + push notifications with smart timing (lead time, timezone, weekday logic). Track delivery → open → action.
- Payments: co-pays, packages, refunds, and receipts; isolate PCI scope; store only tokens.
- Messaging (clinical-safe): secure, role-aware threads; retention policies match your EHR.
- Charting shortcuts: SOAP templates, macros, and quick-pick diagnoses/procedures that actually match how providers document.
- Exports + audit: one-click encounter export, immutable audit trail, and role-based access from day one.
- Vendor-ready plumbing: ID matching and minimal EHR sync so you can expand without a rewrite.
Cut anything that doesn’t accelerate first bookings, faster documentation, or clean payment capture. MVP wins when the front desk spends less time chasing forms and the provider closes notes before dinner.
Advanced Clinical Features for a Chiropractic Mobile App
Add clinical depth only when the basics hum. If you develop chiropractic clinic app capabilities beyond scheduling and notes, pick tools that produce objective data and flow back into the chart.
- Assessment tooling: a modular spine analysis app / posture assessment app that captures calibrated photos or sensor data, with automatic landmarking and error flags. Results save as structured fields for downstream spine assessment and progress graphs.
- 3D spine analysis: reserve for clinics with clear ROI (pre/post visuals that drive adherence or payer documentation). Validate accuracy (device consistency, distance cues, lighting) and disclose limitations; this is adjunctive, not a diagnosis.
- Posture monitoring: lightweight, opt-in tracking via wearables or periodic phone prompts. Translate noise into simple plans (“2× daily mobility set”) and attach to visit notes.
- In-visit helpers: goniometer, ROM timers, image annotation, and templated narrative that drops directly into SOAP.
- Signal, not sparkle: every measurement must map to a decision (treatment change, home program tweak, payer proof). If it can’t alter care, it’s a demo feature.
- Social proof loop: enable compliant patient reviews post-episode; request only after a documented win. Close the loop with provider dashboards showing outcomes and review velocity.
Clinical extras earn their keep when they shorten assessments, clarify plans, and justify care—without trapping data in a sidecar app.
Step-by-Step Development to Create a Chiropractor Application
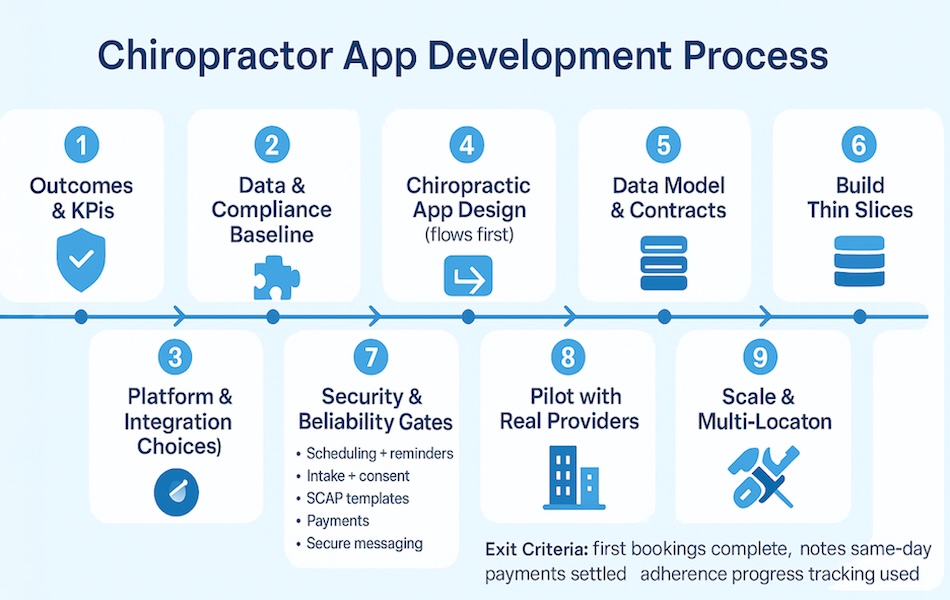
Ship in tight loops, measure everything, and wire compliance from day one. Here’s the order that keeps scope honest and clinics happy.
Step 1: Outcomes and KPIs
Define what “v1 works” means: no-show rate, days-in-AR, note-closure time, patient adherence progress tracking, and review velocity. Pick targets and dashboards before code.
Step 2: Data and Compliance Baseline
Map PHI flows (intake → encounter → billing), consent surfaces, retention windows, and access roles. List vendors needing BAAs. Decide hosting, backups, and incident playbooks now—not during go-live.
Step 3: Platform and Integration Choices
Decide what you assemble vs. build: payments, video, messaging, eligibility. If you’re using a chiropractor app builder (component platform), confirm auth, audit, and consent are shared across modules. Stub a “fake EHR” to unblock development while legal clears the real one.
Step 4: Chiropractic App Design (flows first)
Design the minimum journeys: book → complete patient intake forms/consent forms → visit → pay → follow-up. Use wireflows before pixels. Accessibility, timezone logic, and failure states are part of chiropractic app design, not afterthoughts.
Step 5: Data Model and Contracts
Define core objects (patient, plan, encounter, claim, message) and events (scheduled, arrived, coded, paid). Write API contracts and fixtures. Seed “golden” test scenarios you’ll replay in CI.
Step 6: Build the Thin Slices
Implement vertical slices in this order:
- Scheduling + appointment reminders (SMS/push notifications)
- Intake + consent (mobile, e-sign, field-mapped)
- SOAP templates + quick-codes
- Payments (tokens, refunds, receipts)
- Secure messaging (role-aware, retainable)
Each slice shippable, observable, and permissioned.
Step 7: Security and Reliability Gates
RBAC, audit logging you can query, field-level encryption where it counts, rate limits, and monitoring/alerts. Run privacy threat modeling and basic pentests. Fix the top issues before pilot.
Step 8: Pilot with Real Providers
Roll out to a small cohort (2–3 providers). Train front desk. Track KPIs daily. Instrument every “oops”: reschedules, intake drop-offs, claim rejects. Tighten copy and defaults; don’t add features.
Step 9: Scale and Multi-Location
Only after the pilot hits targets: enable location scoping, shared providers, consolidated analytics, and bulk operations. Add EHR syncs beyond demographics/charts if the ROI is clear.
Step 10: Operate or Hand Off
Runbooks, admin training, error budgets, and a release cadence. If partnering with healthcare app development services, lock a RACI: who owns uptime, integrations, and roadmap.
Exit criterion for v1: first bookings complete without staff back-and-forth, notes close same day, payments settle cleanly, and adherence progress tracking actually gets used.
Technology Stack Recommendations
Clients: Mobile/Web
Ship quickly without boxing yourself in.
- Mobile: React Native (or Flutter) for one codebase; Expo for OTA updates.
- Web Admin: React. Go native modules only when sensors truly matter.
Core Services and Data
Keep the center boring, observable, and swappable.
- Backend: Node/Nest or Python/FastAPI behind a clean service boundary.
- Storage: PostgreSQL for PHI, Redis for queues/caching. Event bus for system events.
Identity and Security
Compliance is an architecture choice, not a checklist.
- Auth: OpenID Connect (Auth0/WorkOS/Cognito) with BAAs, short-lived tokens, scoped roles.
- Audit and Encryption: Queryable audit logs, field-level encryption where it counts, least-privilege IAM.
Communication and Media
Build trust with reliable real-time messaging and safe content delivery.
- Messaging: WebSockets via Ably/Pusher behind an event bus; avoid consumer chat SDKs.
- Exercise videos: HLS streaming on CloudFront + S3 (SSE-KMS), signed URLs, server-side transcodes. No YouTube/Vimeo (PHI risk).
Integrations and Payments
Abstract vendors so swaps don’t become rewrites.
- EHR/Data: HL7/FHIR via Mirth or Redox; contract tests against a fake EHR first.
- Telehealth/Payments: Vonage/Twilio (BAA) and Stripe with PCI isolation.
Ops and Analytics
Instrument day one; guesswork is expensive.
- Infra: AWS + Terraform, monitoring (Datadog/New Relic), errors (Sentry), encrypted backups.
- Analytics: Event tracking into BigQuery/Snowflake; dashboards for ops KPIs and adherence/progress.
Result: a compliant, modular chiropractic practice app you can evolve without heroic refactors.
Compliance That Ships: HIPAA, PCI and Insurance Verification
Treat compliance as architecture, not paperwork. When you build chiropractic mobile application workflows, bake these in:
HIPAA Compliance
Draw hard PHI boundaries (what stores vs. references patient records), short-lived signed URLs for media, and a queryable audit spine (164.312(b)). Kill silent PHI leaks: crash/analytics SDKs, push providers, and verbose logs. Keys live outside the app; device keystores only hold tokens, never payloads.
Related: HIPAA-Compliant App Development Guide
State Retention and Release
Retention isn’t one-size-fits-all; parameterize by state/minor status and make legal holds override deletions. Export that patients can actually use (PDF + machine-readable), with immutable event trails for changes.
PCI DSS without Scope Creep
Keep cards-on-file as tokens; isolate payments so PCI never drags your HIPAA boundary. Never co-mingle payment metadata with clinical notes.
Insurance Verification with Minimal PHI
Use clearinghouses (X12 270/271) behind a proxy; redact payloads in logs, and segregate payer credentials from EHR creds. Eligibility outcomes map to encounters, not screenshots.
Operational Proofs, Not Promises
Immutable backups (object lock), tested restores, RBAC with least privilege, and red-team style checks on role escalation. If it isn’t testable, it isn’t compliant.
If you want the deeper checklist, grab the HIPAA compliance guide—but the above is where most apps actually fail.
Monetizing Your Chiropractor App
Profit flows from clean ops, not price hacks. Wire revenue into the product.
- Upfront capture: In the chiropractor appointment app, take cards-on-file, deposits, and dynamic cancel fees; auto-fill plans/packages at booking.
- Packages & memberships: Prepaid visit banks, auto-renew, and utilization nudges; show remaining credits in-app.
- Payment processing: HSA/FSA, Apple Pay/Google Pay, pay-by-link, split-tender; refunds and chargebacks handled in a PCI-isolated lane.
- Billing integration: Eligibility + real-time estimate → co-pay before visit → post-EOB (Explanation of Benefits) balance nudges; A/R queues with smart retries.
- Chiropractic billing app workflows: Fast charge capture (macros, modifiers), scrub before submit, denials worklists, payer rule library tied to templates.
- Add-ons with receipts: Telehealth follow-ups, posture assessments, and programs sold in-app with transparent pricing and auto-receipt to the chart.
Challenges and Solutions for Developing a Chiropractor Application
The edges—not the features—decide whether a chiropractic patient app and chiropractor scheduling app actually reduce AR days and no-shows. Here’s where builds crack, and what to do instead.
EHR Integration: Identity and Scheduling Authority
Pain: duplicate patients, encounters that won’t reconcile, scheduler tug-of-war.
Solution:
- Make “who owns the schedule” an explicit contract. If EHR is the source of truth, your scheduler is a façade that writes through with idempotent requests and shows authoritative conflicts in-UI.
- Stand up deterministic + probabilistic MPI (Master Patient Index) rules and a human review queue for near-matches; attach evidence (MRN, DOB, payer ID) to every merge.
- Reconcile at the encounter level, not just appointments: post status deltas (arrived, coded, paid) to prevent orphaned visits.
Also Read: How to integrate an EHR into your medical app
Multi-Device Sync Under Real-World Stress
Pain: conflicting edits, lost messages, phantom reminders.
Solution:
- Version every record; expose conflict states in the UI (don’t hide them).
- Outbox pattern on clients; server applies last-write-wins with merge hints for clinical notes.
- Changefeeds (not polling) to keep web/admin and mobile coherent; every write carries an idempotency key.
Offline—Use the Scalpel, Not the Sledgehammer
Safe offline: intake/consent drafts, photo capture, SOAP stubs.
Not offline: eligibility, payments, scheduling (double-book risk).
Solution: encrypted local store with per-field TTLs; queued writes include attestation (who/when/where). On arrival, force draft reconciliation before care starts.
Insurance APIs without Denial Roulette
Pain: 270/271 timeouts, payer quirks, silent duplicates, “estimate vs. reality” drift.
Solution:
- Treat eligibility/claims as jobs with retry + dead-letter queues; strict idempotency by payer.
- Pre-adjudication estimates: show confidence ranges; bake in payer rule packs (required fields, common rejection codes) and surface edits before submit.
- Split secrets: payer credentials isolated from EHR creds; redact payloads at source.
State Differences You Actually Feel
Pain: visit types and coding rules vary; “maintenance” vs. “active care” denials, telehealth parity varies by state/payer.
Solution:
- Load state/payer matrices that govern allowable codes, modifiers, and documentation phrases; fail fast at coding time.
- Gate telehealth slots by location/licensure; block out-of-bounds bookings before they hit the queue.
Staff Management That Prevents Ops Drag
Pain: role drift, brittle availability, rooms idle while providers overbook.
Solution:
- First-class staff management: credential expirations, role scopes, location scoping, and rotation rules.
- Scheduling constraints reflect physics (room, table type, buffer windows); auto-insert documentation blocks to reduce note lag.
- Scorecards: utilization, note-closure latency, rebooking rate—review weekly and tune rules.
Referral Management That Closes the Loop
Pain: inbound faxes/emails vanish; poor conversion; referrers never hear back.
Solution:
- Normalized referral management queue (OCR/fax ingestion, dedupe against existing patients, priority scoring).
- SLA timers drive outreach (call/SMS/email) until first appointment lands; outcomes auto-logged to the chart.
- Post-eval updates to referrers via Direct or portal with templated summaries—compliant and auditable.
Known Traps
- Hidden queues (messages, reminders) without dead-letter handling → silent patient harm. Don’t ship.
- Measurements without units/scales (posture, ROM) → unusable “insights.” Define schemas up front.
- Calendar logic that ignores timezones and daylight shifts → “no-show” mirages. Normalize all times server-side.
- Denial worklists buried in billing → cashflow bleed. Surface them in the admin home with next-action macros.
Bottom line: design rails for identity, synchronization, and operational queues first. Features sit on top of that lattice—or they fall off it.
AI/ML Implementation for Clinical Outcomes
AI earns its keep when it feeds the chart with objective signals, personalizes treatment plans, and trims unnecessary visits—not when it demos well. In a mobile app for chiropractors (or a mobile health app for chiropractic care), start here.
Computer Vision for Posture and Movement
Use pose estimation to turn video into landmarks → joint angles → trendlines. Guardrails: a calibration step (distance cues, lighting checks), automatic occlusion/error flags, and structured outputs that drop into SOAP (not screenshots).
Tie insights to patient education: surface why a stretch matters for pain management, then nudge adherence.
RTM/RPM to Reduce In-Person Visits
Asynchronous check-ins + guided home exams can safely replace many follow-ups. In our RTM build, computer-vision exams at home plus clinician dashboards drove up to 50% fewer in-person visits, while cutting clerical time ~80% via automated data capture and workflows.
That’s the pattern to replicate for chiropractic: exam kits at home, thresholds and alerts in the admin, and clear escalation paths to in-clinic care.
Related: Remote Patient Monitoring App Development Guide
Goniometric Measurements from Video
Angle math matters more than models. Use stable keypoint sets (e.g., hip–knee–ankle) and consistent camera geometry; compute ROM deltas against a patient baseline, not generic normals.
Present angles alongside function (“sit-to-stand reps up 20%”) to make plan changes obvious. This is how we delivered joint-angle metrics from standard phone video and charted progress over time.
Model Placement: Cloud vs. Edge
- Cloud inference: Faster R&D, centralized updates, heavier privacy work (tokenized media, short-lived URLs), and solid connectivity required. We chose cloud in production to keep model iteration rapid and avoid app-store release cycles for every tweak.
- Edge inference: Lower latency and better offline resilience, but larger app bundles, device variability headaches, and slower rollouts. Reserve for kiosk-like setups or when video never leaves the device.
Case in Point (transferable to chiropractic)
Allheartz—an RTM platform we built—combined pose recognition, video-based goniometry, clinician dashboards, and plan templates to deliver measurable outcomes:
- up to 50% fewer in-person visits
- ~80% less clerical drag, and injury-risk reductions in sports contexts
Stack: TensorFlow/MoveNet, React Native, web admin, cloud inference. The architecture maps 1:1 to chiro: at-home exams, structured ROM metrics, and plan-driven follow-ups that escalate only when needed.
A mobile health app chiropractic practices can trust should turn video into objective measures that flow into the chart and actually change care.
Build vs. Buy Decision Framework
Speed is easy; control is expensive. Pick the base for your chiropractic clinic software by deciding what you must own (data model, workflows) vs. what you can rent (telehealth, payments).
Quick Comparison
| Dimension | Custom Build | White-Label Platform | SaaS Platform |
| Time-to-market | 6–12 months (teams + pilots) | 2–8 weeks (theming + config) | Days–2 weeks (setup) |
| Data architecture & ownership | You design it; full control of patient records and events | Vendor schema; exports vary by vendor | Fixed schema; API/webhook quality varies |
| Workflow control | Unlimited (you own code) | High within vendor rails | Moderate; fit to product |
| EHR/payor integrations | Deep, bespoke | Usually shallow or prebuilt | Limited to vendor roadmap |
| Chiropractic telehealth app / virtual consultations | You choose stack & retention | Often bundled; configurable | Bundled; policy fixed by vendor |
| Inventory tracking & ancillary ops | Tailored (rooms, tables, supplies) | Add-on or workaround | Often minimal or generic |
| Compliance surface | You own HIPAA/PCI ops | Shared with vendor (BAA required) | Mostly vendor; you still govern use |
| TCO pattern | CapEx heavy; lower marginal cost at scale | Mid; platform fees + change orders | OpEx; subscription + overages |
| Lock-in risk | Low (you own code & infra) | Medium–High (templates, SDKs, data export limits) | High (data model + feature roadmap) |
| Examples/notes | Great for multi-location complexity, IP | Faster brand control; check export rights | Fastest path; least control |
Vendor Lock-In—Read Before You Click “Publish”
Platforms like Shoutem or GoCanvas ship fast, but rails are real: template limits, closed components, and uneven data egress. Require: (1) full JSON/NDJSON exports for patients/encounters/payments/audit logs, (2) event webhooks, (3) BAA covering all subprocessors, (4) contract language for migration assistance.
When Custom Development Actually Makes Sense
- Multi-location practices with shared providers, nuanced scheduling, and consolidated reporting.
- Unique IP in treatment protocols, plan logic, or outcomes scoring you’ll defend or license.
- A roadmap that needs deep EHR/payor plumbing, or advanced ops (referrals, utilization, inventory tracking).
- Eventual acquisition or enterprise partnerships where owning the data model/audit trail increases valuation.
- You need a telehealth layer you can truly govern (recording retention, evidence capture) rather than “whatever the vendor ships.”
Related: Custom App Development
Pragmatic Path (Hybrid)
Start on SaaS for bookings and virtual consultations, keep the data exhaust (events → warehouse), then peel off the high-ROI flows into a custom service. That turns “buy vs. build” into “buy then build,” with a controlled exit from lock-in when the math supports it.
Development Cost Breakdown
Grounded ranges for U.S. small-practice builds (HIPAA grade), distilled for planning—not sticker shock.
Budget Bands
- Feasible window: $25k–$100k for constrained scope.
- Typical reality (HIPAA-grade): ~$40k–$150k once you add telehealth or light EHR sync.
- Heavy integrations: $100k–$200k when multiple payers/EHRs or complex workflows enter the chat.
Where the Dollars Go
- Auth & roles: $4k–$10k
- Profiles/onboarding: $10k–$15k
- Scheduling: $3k–$8.5k
- Push/notifications: $1k–$5k
- Secure chat/messaging: $5k–$10k
- Payments (per method): $3k–$7k
- Geolocation/visit logistics: $7k–$15k
- Telehealth: $10k+
- EHR/EMR integration (per vendor): $25k+
Heuristic: anything that touches identity, money, or clinical evidence costs more than it looks—because testing and auditability aren’t optional.
What Fits in a Lean MVP
A clinic-ready strip-down—scheduling + payments + reminders (no EHR/telehealth)—typically lands ~$40k–$70k in healthcare due to HIPAA, threat modeling, and QA overhead. Ship this when the goal is bookings, clean capture, and fewer no-shows.
What Pushes You Up a Bracket
Add telehealth or basic EHR sync and the total moves to ~$80k–$150k. You’re paying for encryption boundaries, retention policies, consent surfaces, and integration test matrices—i.e., real risk reduction, not “extra features.”
Related: Telehealth App Development
Ongoing (Run-Cost) Reality
Plan ~20–45% of build/year for maintenance, OS/security updates, monitoring, and minor feature work. Third-party services (video, payments, hosting) commonly add ~$500–$5,000/mo depending on volume.
Timelines (So You Can Staff It)
- Scheduling-only: 6–12 weeks
- EMR/records modules: 12–24 weeks
- HIPAA small-practice MVPs: ~4–6 months (case patterns show ~3–6 months when scope holds)
Scope Multipliers (Quiet Budget Killers)
- Practice analytics dashboards (retention, AR, cohorting) expand the data model and pipeline testing.
- Multi-location support multiplies roles, permissions, and scheduling matrices—assume higher QA and change-management.
Sanity check: If someone quotes “HIPAA + EHR + telehealth” for $20k, they’re skipping security and validation. Politely decline and protect your runway.
North-Star Metrics for Chiro Apps
Measure what pays the rent: adoption, attendance, satisfaction, revenue per patient, time per visit, and staff load—wired to event streams from day one so improvements are provable, not vibes.
- User adoption rate: MAU ÷ active patient panel; track login/open + completed key flows (intake, booking).
- Appointment no-show reduction: (Baseline no-show − post-launch) ÷ baseline; source = scheduler/EHR status.
- Patient satisfaction scores: CSAT/NPS after each encounter; tie responses to encounter IDs for cohorting.
- Revenue per patient increase: Collected revenue ÷ unique patients; segment by payer/visit type to isolate lift.
- Time saved per appointment: Note-closure time and admin touches per visit (timestamps + event logs).
- Staff efficiency: Front-desk contacts per booking, reschedule loop count, claim rework rate, first-pass acceptance.
Set these up as always-on dashboards; if a metric can’t be computed from events, the feature isn’t done.
How Topflight Can Help You Build an App for a Chiropractor Clinic
Healthcare App Expertise
Product-first, code-second. We scope to workflows that move KPIs (no-shows, AR days, note-closure time), ship thin vertical slices, and prove value in pilot before scaling.

HIPAA-Compliant Development
Compliance is architectural: PHI boundaries, RBAC aligned to real roles, queryable audit logs, short-lived media links, and vendor BAAs. We threat-model early so security isn’t a retrofit.
EHR and Device Integrations
From HL7/FHIR to wearables, we design contract-tested adapters and late-bind the real vendor to avoid identity collisions and orphaned encounters. See our EHR approach for depth: Topflight EHR Integration.
Applied AI That Improves Outcomes
Pose estimation, video goniometry, triage scoring—used only where they change decisions (treatment plans, pain management, adherence). Cloud or edge, we pick the right placement and ship safely. Learn more: Topflight AI services.
Post-Launch Support and Scaling
Runbooks, monitoring, and a release cadence baked in. As you add locations, programs, or analytics, we evolve the data model—no CSV duct tape.
Want a straight answer on scope, risk, and the fastest path to pilot? Let’s talk. We’ll outline a pragmatic plan—SaaS, hybrid, or a custom chiropractor app—and the milestones to hit ROI without drama. Book a consult and get an opinionated roadmap you can execute.
Frequently Asked Questions
What belongs in a chiropractic MVP?
Scheduling, mobile intake and consent, payments, reminders, secure messaging, and basic charting that matches how providers actually document.
Do I need EHR integration on day one?
Not necessarily; start with clean identity and exports, then add demographics or encounter sync when the ROI clears and legal/BAAs are in place.
How long does it take to ship a usable V1?
A lean, HIPAA-grade MVP commonly lands in a few months if scope holds; scheduling-only builds can be faster.
How do you keep HIPAA and PCI from colliding?
Tokenize cards, isolate payment systems from clinical data, and never co-mingle payment metadata with notes.
How do I avoid vendor lock-in with white-label platforms?
Require full data exports, webhooks, signed BAAs for all subprocessors, and a contractual migration clause before you launch.
Where does AI actually help in chiropractic care?
Pose estimation and video goniometry that produce structured ROM metrics, tie into treatment plans, and trigger clear follow-ups or escalations.
What metrics prove the app is working?
Adoption and completion rates, no-show reduction, time to note closure, revenue per patient, and first-pass claim acceptance.