💡 Quick Pricing Summary (Epic EHR, 2026)
-
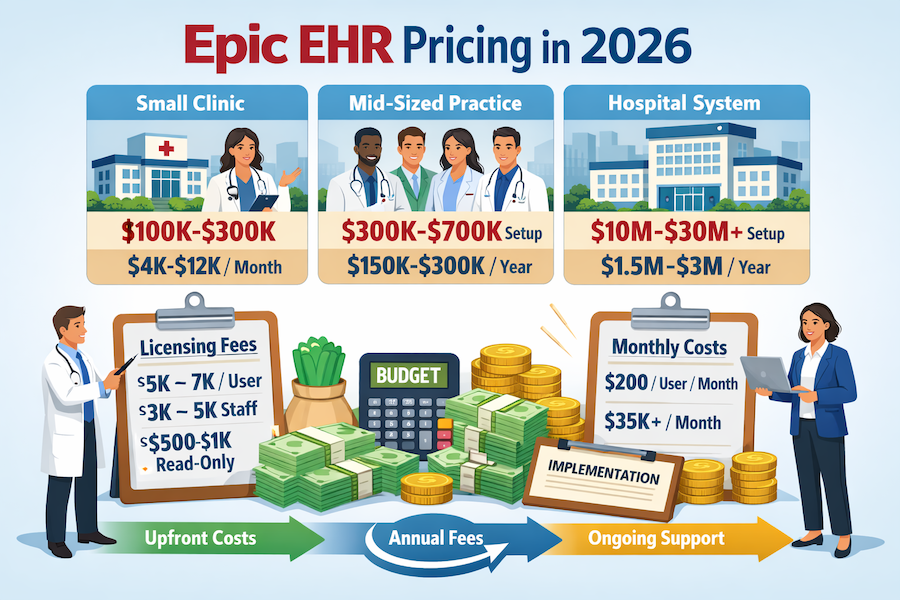
Typical upfront ranges: $100K–$300K (small clinic) → $10M–$30M (hospital/health system).
-
Recurring spend signals: $4K–$12K per month (small clinic equivalent) or $1.5M–$3M per year (hospital/health system support/maintenance).
-
Pricing units you’ll see in quotes: per user, per bed, per location, plus subscription per month for hosted deployments.
-
Anchor numbers to sanity-check line items: $5K–$7K per user (physician license), $200 per user per month (hosted starting point), and enterprise hosted can reach $35K+ per month.
If Epic were a luxury car, it’d undoubtedly be a Lamborghini: sleek, powerful, and outrageously expensive. And just like when considering that exotic car, healthcare executives often find themselves asking: “How much does Epic cost?”
It’s not just curiosity—it’s a survival instinct. In 2026, with razor-thin margins, mounting regulatory pressures, and increasingly demanding patients expecting seamless experiences, guessing is no longer an option. You need exact numbers, clear insights, and actionable strategies to leverage Epic without breaking the bank. Consider this guide your financial GPS—no fluff, no jargon, just the precise, actionable insights you need to steer confidently through the maze of Epic pricing and implementation.
Additionally, whether you’re gearing up for regulatory attestation or carefully budgeting for a clinic deployment, knowing the granular details upfront helps ensure you get maximum value without unwelcome financial surprises down the road.
Key Takeaways:
- Epic pricing scales significantly with organization complexity—smaller clinics may face prohibitively high per-user costs, making detailed pre-implementation analysis crucial.
- Understanding and proactively managing hidden implementation expenses—training, maintenance, upgrades—can dramatically lower the total cost of Epic, protecting your ROI from unexpected financial strain.
- Leveraging AI-driven optimizations within Epic early can directly cut operational overhead and improve clinical productivity, significantly offsetting the initial high cost of Epic EHR.
Table of Contents:
- Understanding Epic EHR Pricing in 2026
- Epic EHR Cost Breakdown
- Epic EHR Implementation Expenses: The True Cost of Getting Epic Up and Running
- Key Factors Influencing Epic EHR Pricing: Navigating Your Investment Wisely
- Epic EHR vs. Competitors: A Cost Comparison
- Maximizing ROI with Epic EHR in 2026: Turning Costs into Strategic Advantages
- How Topflight Keeps Epic Projects on Budget
- Is Epic EHR Worth the Investment in 2026?
Understanding Epic EHR Pricing in 2026
Epic EHR pricing (and Epic EMR pricing) is not a public checkout page. There’s no official price list you can screenshot and take to procurement. What you can get is a defensible estimate based on how Epic’s fee structure typically works: upfront licensing fees + implementation + ongoing annual fees for support (or a hosted subscription billed per month).
If you’re comparing solutions or planning a replacement of a legacy system, the only sane way to budget is to break Epic down into “what you pay once” vs “what you pay forever.”
What Does Epic EHR Cost in 2026?
Here’s the “definitive enough to budget” view of Epic EHR costs, by organization size:
-
For a small clinic: $100,000–$300,000 initial setup, then $50,000–$150,000 ongoing yearly costs. That commonly translates to $4,000–$12,000 per month once you spread operating costs out.
-
Mid-sized practices (4–10 providers): $300,000–$700,000 initial setup, plus $150,000–$300,000 in recurring annual expenses (maintenance + support + operating overhead).
-
Hospitals & health systems: often $10M–$30M upfront, with $1.5M–$3M in annual fees for maintenance/support (and that’s before you count internal staffing and broader transformation costs).
Translation: Epic is rarely “an IT purchase.” It’s an investment program that reshapes workflows across organizations, not just one medical facility.
Epic EHR Pricing Calculator and Quick Reference
Epic won’t hand you a calculator. So make your own breakdown using pricing “units” Epic and buyers actually talk in:
Quick reference (common pricing units):
-
Per user licensing (providers vs staff vs read-only)
-
Per bed licensing for hospitals (a proxy for facility scale)
-
Per month subscription charges for hosted setups
-
Per location rollouts (multi-site clinics, satellites, affiliates) — this is where costs sneak up fast during implementing, because each site adds training, build/config, interfaces, and go-live support.
Use this mini-calculator framing in internal planning:
-
Upfront: license + implementation services + training + (if on-prem) infrastructure
-
Ongoing: maintenance/support annual fees (often modeled as a % of license) or subscription billed per month
-
Internal ops: staffing + upgrades + interfaces/integration support
That structure is boring—which is why it works in real budgeting meetings.
How Much Does Epic Cost Per User?
Epic rarely behaves like “$X per seat.” But the research ranges are still useful for planning:
-
Physician license: $5,000–$7,000 per user (one-time license fee range)
-
Other clinical staff: $3,000–$5,000 per user
-
Read-only users: $500–$1,000 per user
This is why “let’s give everyone access” is the fastest way to inflate Epic software cost. The more disciplined your role design is before implementing, the less painful your final Epic EHR pricing ends up being.
Epic EHR Monthly Subscription Costs Explained
There are two common “monthly” realities in Epic budgets:
-
Hosted/subscription model: starts around $200 per user per month for basic setups, and can scale to $35,000+ per month for larger deployments.
-
Licensed/on-prem model: you pay big upfront, then recurring maintenance is often modeled at roughly ~20% of the initial licensing cost per year (a huge line item people forget until it’s too late).
So if someone asks, “What’s the average Epic cost?” the only honest answer is: the average depends on your contract model (license vs subscription), scope, and scale—but the budgeting math always reduces to the same breakdown: upfront + annual fees + internal support.
Epic EHR Cost Breakdown
💡 Quick Cost Summary (Epic EHR Cost Breakdown)
-
Upfront (typical): $100K–$300K (small clinic) • $300K–$700K (mid-sized practice) • $10M–$30M+ (hospital/health system).
-
Ongoing (typical): $4K–$12K per month (small clinic equivalent) • $150K–$300K per year (mid-sized practice) • $1.5M–$3M per year (hospital/health system).
-
Licensing anchors: $5K–$7K per user (physician) • $3K–$5K per user (staff) • $500–$1K per user (read-only) • $500–$1K per bed (hospital sizing).
-
Maintenance baseline: ~15–20% of license cost per year (often modeled ~20%).
Now let’s break those totals into clean, quotable parts: licensing ranges, 2026 quick facts, and small-vs-large comparisons.
Epic EHR costs range from roughly $100,000–$300,000 upfront for a small clinic to $10M–$30M+ for a hospital system, plus ongoing costs that can run from $4,000–$12,000 per month (small clinic equivalent) to $1.5M–$3M per year (hospital/health system), depending on licensing, hosting, and support model.
Epic EHR Licensing Cost Summary
|
Licensing unit |
Typical planning range |
Notes (what this usually covers) |
|---|---|---|
|
Physician license (per user) |
$5,000–$7,000 |
One-time licensing estimate per physician user. |
|
Clinical staff license (per user) |
$3,000–$5,000 |
Nurses/therapists/other staff user licenses. |
|
Read-only license (per user) |
$500–$1,000 |
“View access” is typically not free. |
|
Hospital metric (per bed) |
$500–$1,000 per bed |
A common sizing metric for hospital licensing estimates. |
|
Annual maintenance (self-hosted license) |
~20% of initial license cost / year |
Maintenance/support fee planning baseline. |
Epic Pricing Quick Facts for 2026
|
Epic EHR pricing fact (2026) |
Practical number to use in budgets |
|---|---|
|
Small clinic initial setup (all-in starting point) |
$100,000–$300,000 upfront |
|
Small clinic ongoing (spread to monthly equivalent) |
$4,000–$12,000 per month |
|
“Minimal” small-clinic scenario (rare; typically hosted/limited) |
~$1,200 per month (low-end signal) |
|
Mid-sized practice (4–10 providers) initial setup |
$300,000–$700,000 upfront |
|
Mid-sized practice recurring annual expenses |
$150,000–$300,000 per year |
|
Hospital/health system upfront (enterprise) |
$10M–$30M+ upfront |
|
Hospital/health system ongoing (maintenance/support) |
$1.5M–$3M per year |
|
Hosted subscription starting point (small practice) |
~$200 per user per month |
|
Hosted subscription at scale (enterprise signal) |
$35,000+ per month |
|
Internal Epic support staffing (common add-on to “software cost”) |
$150,000–$500,000 per year |
Cost Comparison: Small vs. Large Organizations
|
Cost component |
For a small clinic |
For a mid-sized practice (4–10 providers) |
For a hospital system |
|---|---|---|---|
|
Upfront program cost (setup + build) |
$100K–$300K |
$300K–$700K |
$10M–$30M+ |
|
Ongoing operating cost (recurring) |
$50K–$150K / year (≈ $4K–$12K per month) |
$150K–$300K / year |
$1.5M–$3M / year |
|
Licensing pattern |
Mostly per user (providers + staff + read-only) |
per user + broader module scope |
Often modeled by per bed and enterprise scope |
|
Maintenance model (if self-hosted) |
~20% of license / year |
~20% of license / year |
~20% of license / year |
|
Hosted subscription option |
Can start around $200 per user per month; rare low-end ~$1,200/month signals exist |
Usually grows into higher recurring fees as scope expands |
Can reach $35K+ per month and beyond |
|
“People cost” often omitted from software quotes |
$150K–$500K/year internal support staffing can apply as complexity grows |
Same dynamic—more users/modules = more admin/support needs |
Often large dedicated Epic teams (material operating expense) |
How to sanity-check an Epic quote using the tables above
-
Classify your org (small clinic vs mid-sized practice vs hospital system) and treat that row as your “budget envelope.”
-
Ask which pricing unit is driving the quote: per user (providers/staff/read-only) or per bed—then compare the line items to the Licensing Cost Summary ranges.
-
Separate one-time costs (setup/build) from recurring costs (maintenance, hosting, support) and convert recurring costs to a single annual number for apples-to-apples comparison.
-
Check whether maintenance is modeled as ~20% of license per year (common baseline) or buried inside another line item.
-
Verify what’s included in “support”: if you’ll still need internal Epic admins/analysts, add a staffing line (often $150K–$500K/year) so you don’t underbudget operating cost.
-
If the quote is “surprisingly cheap,” confirm scope: number of users, modules, per location rollout, integrations, training, and go-live support—this is where the real spend tends to hide.
Epic EHR Implementation Expenses: The True Cost of Getting Epic Up and Running
💡 Quick Implementation Cost Summary (Epic EHR)
-
Total implementation cost (typical): $100K–$300K upfront (small clinic) → $10M–$30M+ upfront (hospital/health system).
-
Big upfront buckets: licensing + installation ($2M–$10M+), infrastructure ($2M–$10M on-prem), migration ($1M–$5M), training ($2M–$10M).
-
Run-rate costs to budget (every year): maintenance fees (~20% of license / year) + internal support staffing ($150K–$500K/year).
-
Most-missed budget line items: data cleanup before migration, testing/UAT, go-live support, post-go-live optimization (these drive “hidden costs” and operating costs).
Now let’s unpack where implementation budgets actually go—so you can spot under-scoped quotes before they become expensive surprises.
Implementing Epic is more than just software installation; it’s a strategic transformation that carries significant financial implications. Decision-makers must thoroughly understand the EHR implementation cost to ensure realistic budgeting and avoid painful surprises later on. Let’s unpack these critical costs.
Total Cost of Epic EHR Implementation
The total cost of Epic EHR implementation is typically the sum of (1) startup licensing + installation, (2) infrastructure, (3) migration, (4) training, and (5) ongoing operating costs such as maintenance fees and support staffing. This is the most practical overview for budgeting the true cost of Epic EHR across medical software systems.
Cost components (typical planning ranges):
-
Software licensing + installation: $2M–$10M+ for large-scale hospital projects
-
Hardware & infrastructure (on-premise): $2M–$10M additional startup investment
-
Data migration: $1M–$5M depending on legacy complexity
-
Training: $2M–$10M (large health systems; smaller orgs spend less but still material)
-
Annual maintenance fees + upgrades: often modeled around ~20% of initial licenses (annual fees)
-
Support staffing: $150,000–$500,000 annually (internal team)
Rule of thumb: If a quote only covers software and ignores migration, training, and operating costs, it’s not a total-cost estimate—it’s a partial invoice.
Hidden Costs of Epic EHR: Complete List
Hidden costs aren’t optional; they’re the part of the Epic EHR price that shows up after go-live—right when everyone is out of patience and out of budget.
Hidden costs checklist:
-
Training time + backfill coverage (lost productivity during training)
-
Workflow redesign + change management (not just IT work; clinical operations)
-
Interface/integration work (labs, imaging, billing, portals, identity, etc.)
-
Data cleanup before migration (garbage-in, expensive-garbage-out)
-
Testing + validation cycles (UAT, regression, downtime planning)
-
Go-live support (at-the-elbow support, extended hours)
-
Maintenance fees & upgrades (recurring; required for security/compliance)
-
Internal support staffing (admins/analysts/reporting/operations)
-
Reporting/analytics rebuild (dashboards rarely “port over”)
-
Post-go-live optimization (the “we’ll fix it later” backlog)
The hidden costs are where the operating costs live.
How to Budget for Epic EHR Implementation
A budget that survives contact with reality separates startup costs from ongoing subscription / annual run-rate and forces a clear cost-benefit analysis of cloud-based vs on-premise technology deployments.
Budgeting steps (simple, defensible):
-
Define scope: medical facility size, number of users, modules, and locations
-
Pick a deployment model: cloud-based subscription vs on-premise systems
-
Break costs into buckets: licensing/installation, infrastructure, migration, training, support
-
Convert everything to a single timeline: upfront (Year 0–1) vs operating costs (Years 2–5)
-
Add contingency: reserve for integration, data cleanup, and go-live support (the usual “unknown knowns”)
-
Track a “run-rate” number: annual maintenance fees + support staffing + upgrade effort
-
Don’t hide people-cost: internal support is part of the system’s true cost of Epic EHR
Upfront Costs: Software, Hardware, and Infrastructure
The cost of Epic upfront isn’t just about purchasing software—it’s about preparing your entire infrastructure. Here’s an overview of what goes into these substantial startup expenses:
-
Software installation: Initial licensing can easily range from $2 million to over $10 million for large-scale hospital projects, making it one of the heaviest line items in your electronic health records implementation budget.
-
Hardware & infrastructure: Epic’s demands on medical software systems are substantial, often requiring extensive server and network upgrades. Budget an additional $2–10 million for infrastructure investments if opting for an on-premise deployment.
-
Data migration: Transferring existing medical data into Epic isn’t trivial. Allocate between $1–5 million depending on legacy system complexity and the volume of records migrated.
Practical tip: Cloud-based Epic deployments can mitigate some hardware investments, shifting upfront costs into manageable monthly fees under a subscription model.
Hidden Costs: Training, Maintenance, and Upgrades
Don’t let hidden costs derail your Epic implementation. Decision-makers often underestimate these essential yet overlooked components:
-
Training: Effective staff training isn’t optional—it’s critical. Expect $2–10 million in initial training expenses for larger health systems. Ongoing refreshers and onboarding new staff add continuous operating costs.
-
Maintenance fees & upgrades: These typically represent about 20% annual fees on initial licenses. Regular software updates and EHR system upgrades are essential for compliance, security, and functionality, often costing large hospitals up to $2 million annually.
-
Support staffing: A dedicated internal IT team to manage and maintain your Epic system can cost between $150,000–$500,000 annually, depending on team size and scope of responsibilities.
Challenge: Many organizations initially overlook training and support expenses, creating financial strain post-implementation.
Opportunity: Early planning, clear budgeting, and dedicated resources for training and support significantly improve system adoption rates and reduce downtime, maximizing ROI.
Cloud-Based vs. On-Premise Deployment: Weighing Your Options
Choosing between cloud-based solutions and on-premise technology deployments has major implications for the overall Epic EHR price:
-
Cloud-based: Lower upfront costs but higher long-term subscription expenses. Suitable for smaller practices or organizations without extensive IT infrastructure. Ongoing fees are predictable and scalable.
-
On-premise: Significant upfront costs, but potentially lower ongoing cost of Epic EHR in the long run—especially advantageous for large healthcare systems with existing robust IT resources.
Recommendation: Conduct a thorough cost-benefit analysis factoring in total cost of ownership over five to ten years. For many mid-size to large organizations, on-premise solutions still offer superior long-term value, provided they have robust internal IT capacity.
Key Factors Influencing Epic EHR Pricing: Navigating Your Investment Wisely
💡 Quick Drivers Summary (Epic EHR Pricing)
-
Why Epic medical records cost swings so widely: Epic EMR cost scales with organization complexity, number of sites, module scope, and the depth of integration and workflow change your management team signs up for. Chief medical officers must consider the operational burden, not just the contract.
-
Top price drivers (highest impact): org complexity → multi-site rollout → module scope → integration depth → customization level → user/role design (support load) → hosting model.
-
What pushes pricing up fastest: trying to integrate a health app with Epic while also attempting to integrate Allscripts EHR (or other legacy systems) without a tight interface plan and experienced EHR integration services.
-
How to reduce Epic EHR costs without self-sabotage: standardize workflows before customizing, phase rollouts, design roles aggressively, and prioritize adopting AI features that measurably avoid medical errors and improve billing outcomes (real “value for money,” not a demo).
Now let’s zoom in on the drivers you can’t change versus the levers you actually control.
If you’ve gotten this far, you’re already aware that Epic isn’t just software—it’s a strategic business decision. But beyond the obvious line items, multiple nuanced factors significantly affect Epic EHR pricing. Let’s dive into these factors so you understand precisely how they’ll shape your bottom line and practical outcomes.
Why Does Epic EHR Cost So Much?
Epic EHR pricing is high because Epic is typically deployed as an enterprise-wide platform (not a single tool), and total cost scales with organization size, modules, and deployment model, plus the implementation and ongoing support needed to keep the system reliable.
In practice, Epic medical records cost isn’t standardized. That’s intentional: most buyers are purchasing a bundle of capabilities and services that touches clinical, operational, and revenue workflows. Decision-makers—especially chief medical officers—must consider not just the upfront contract, but the downstream management burden of training, optimization, governance, and continuous change across workflows.
What Drives Epic Pricing Higher or Lower?
These are the factors that swing Epic pricing the most (and they usually compound—because of course they do):
-
Organization size & complexity (scale tax): larger entities typically require more modules, more users, more build, and more change management—so costs rise accordingly.
-
Multi-site management: every additional facility/location tends to add rollout effort (build, training, go-live coordination), which increases the cost curve faster than teams expect.
-
Deployment model (hosted vs on-prem): hosted subscription models shift cost into ongoing monthly spend; on-prem tends to be heavier upfront but can compare better over a longer horizon at scale.
-
User count + role design: more users (and less disciplined permissioning) typically increases licensing and internal support needs.
-
Integration and customization depth: the more you try to reproduce legacy behavior via custom build and custom interfaces, the more you pay—often in both cash and timeline.
KPI Alert: A complex multi-site rollout can land in eight-figure territory; one benchmark cited is upwards of $80 million for a 500-provider health network when all costs are included.
Where this gets real: costs rise quickly when attempting to integrate a health app with Epic or even to integrate Allscripts EHR alongside other legacy systems—because integration is rarely “just plumbing.” It rewires operations.
Epic Cost Factors Ranked by Impact
-
Organization size & operational complexity (the primary multiplier)
-
Number of locations + rollout sequencing (multi-site management overhead)
-
Module scope (what you buy vs what you actually implement)
-
Integration depth (interfaces, data flows, validation across systems)
-
Customization level (standard workflows vs bespoke workflows)
-
User count + permission model discipline (who gets what access)
-
Deployment model (hosted subscription vs on-prem tradeoffs over time)
-
Optimization posture post go-live (whether you fund continuous improvement or let the system fossilize)
How to Reduce Epic EHR Costs
You don’t “make Epic cheap.” You make your Epic EMR cost predictable—and you stop paying for decisions you didn’t mean to make.
Cost-reduction moves that actually work:
-
Standardize first, customize later: lock core workflows before you start funding “preferences.”
-
Treat integration as a product (not a task): prioritize only the interfaces that reduce operational friction or unlock revenue impact; use specialized EHR integration services when complexity is high so you don’t pay twice—once for build, then again for cleanup.
-
Be ruthless about roles: define who truly needs full access; keep read-only/read-mostly roles tight so licensing and support don’t balloon.
-
Phase the rollout: reduce multi-site chaos by sequencing locations and hardening the model before replication.
-
Use AI where it buys down operating cost: adopting targeted AI-driven analytics inside Epic can help avoid medical errors and improve billing performance—two places where “value for money” is measurable (not vibes).
Actionable Insight: Prioritize AI features that directly affect clinical accuracy, billing efficiency, and patient engagement—those are the levers most likely to offset ongoing operating cost without adding unnecessary implementation complexity.
Epic EHR vs. Competitors: A Cost Comparison
Let’s get real—choosing an EHR system isn’t just about ticking regulatory boxes; it’s about picking the solution that delivers the best blend of capability, scalability, and financial sense for your healthcare organization.
While Epic EHR is undoubtedly powerful, its significant Epic EMR price warrants a clear-eyed ehr/emr systems comparison. Here’s a concise yet comprehensive look at how Epic stacks up against its primary competitors in terms of pricing, ROI, and long-term strategic fit.
Epic vs. Cerner: Pricing and Value in 2026
In the heavyweight arena of hospital EHR solutions, Epic and Cerner (Oracle Health) continue their dominance—but their pricing and strategic value propositions differ significantly:
Licensing & Subscription Costs
Epic: Customized upfront contracts or subscription pricing typically starts at about $1,200 per user or a minimum of around $500,000 for substantial deployments.
Cerner: More predictable, cloud-based pricing models, beginning around $25 per user monthly, making Cerner substantially more approachable for mid-sized or community-focused health systems.
Implementation Expenses
Epic: Implementation projects often exceed $500K even for mid-sized organizations, reaching into tens of millions for larger institutions (for context, Northwell Health’s recent Epic rollout exceeded $1 billion).
Cerner: Implementation typically ranges from $150,000–$300,000 for mid-sized hospitals—noticeably less than Epic.
Maintenance and Support
Epic: Annual support generally equals about 15-20% of licensing fees (hundreds of thousands annually for large hospitals).
Cerner: Lower annual maintenance costs, often around $100,000 annually for average-sized hospitals.
Practical Insight
Epic offers superior enterprise capabilities and scalability, but Cerner often provides quicker ROI due to lower upfront and ongoing costs. Organizations must evaluate their actual need for Epic’s broader functionality before committing.
Epic vs. Allscripts: Which Offers Better ROI?
If your organization’s priorities lean more towards cost sensitivity and ease of adoption, Allscripts (Veradigm) might be a smarter choice. Here’s why:
Pricing Structure & Service Charges
Allscripts: Subscription plans often start around $500–$1,500 per provider per month, ideal for smaller practices aiming to avoid Epic’s significant upfront cost and service charges.
Epic: Generally, custom-quoted pricing scales significantly higher, particularly for larger implementations, making it less practical for tight-budget clinics.
Implementation & Scalability
Allscripts: Small practices report implementation costs around $75,000, significantly lower than Epic’s six-figure minimums. Even a 300-bed hospital spent approximately $2 million on Allscripts compared to tens of millions for an equivalent Epic rollout.
Epic: Scalable upwards and well-suited for large integrated networks, but often prohibitive for smaller organizations.
User Experience & Efficiency Gains
Allscripts: Known for a simpler interface with quicker onboarding, meaning reduced training overhead and less operational disruption.
Epic: Offers deeper integration and advanced analytics but demands significant training resources and higher initial complexity.
Practical Takeaway
Allscripts provides rapid implementation, lower service charges, and quick adoption—perfect for smaller to mid-sized groups prioritizing quick wins and straightforward usability. However, for comprehensive, integrated medical history tracking and deep interoperability, Epic is unmatched in the long run.
Deciding Between Epic, Cerner, and Allscripts
When evaluating which vendor fits your organization’s strategic objectives, consider these critical dimensions:
| Factor | Epic | Cerner | Allscripts |
| Initial Investment | High ($500K – millions) | Moderate ($150K – $300K) | Lower ($75K – $2M) |
| Annual Support Costs | High (15-20% licensing) | Moderate (~$100K annually) | Moderate (varies widely) |
| Scalability | Best for large hospitals | Scalable (mid-large) | Ideal for small practices |
| Ease of Adoption | Complex, extensive setup | Moderate complexity | Easier, faster adoption |
| ROI Horizon | Long-term, strategic | Mid-term, balanced | Short-term, immediate gains |
Ultimately, while Epic might lead in capability and enterprise-scale solutions, decision-makers must evaluate carefully whether the premium is justified for their specific scenario, or if Cerner or Allscripts present stronger financial logic, especially in smaller or medium-sized environments.
Maximizing ROI with Epic EHR in 2026: Turning Costs into Strategic Advantages
In healthcare, ROI isn’t just about financial returns—it’s about enhancing patient outcomes, boosting efficiency, and yes, making your CFO smile at quarterly reports. One of the most common questions we hear from healthcare decision-makers is: “How much does Epic EHR cost?”
The truth is, Epic isn’t cheap, and achieving strong ROI demands strategic thinking and proactive planning. Let’s unpack exactly how to make every dollar spent on Epic count, leveraging practical solutions and emerging technologies.
Additionally, whether you’re preparing for regulatory attestation or simply budgeting for a clinic, it’s essential to dive into the granular details of Epic’s cost structure to avoid surprises and maximize the value you derive from this robust platform.
AI-Powered Workflow Enhancements: Streamlining for Efficiency
Epic implementations provide a golden opportunity to enhance workflows through integrated AI solutions. By incorporating advanced AI-driven features into your healthcare app development strategy early, you can significantly cut operational overhead, increase clinician productivity, and directly impact patient outcomes.
Key Opportunities:
- Automated Documentation: Voice-driven AI reduces clinician documentation time by up to 45% per year, freeing medical staff for direct patient care.
- Clinical Decision Support: AI-driven predictive analytics embedded in Epic can drastically decrease preventable readmissions, generating substantial savings annually.
Challenges & Limitations:
- High initial investment for AI modules may intimidate smaller clinics or private practices.
- Resistance from clinicians if AI integration is perceived as disruptive.
Practical Advice:
Start small—implement high-impact, low-disruption AI tools first (like speech-to-text) and expand into predictive analytics as user comfort grows.
Reducing Hidden Costs with Smart Implementation: Efficiency at Scale
Hidden expenses—often lurking within training, customization, and system support—can sabotage Epic’s value proposition if not proactively managed. Strategic planning is critical to avoiding these budgetary black holes.
Actionable Strategies from our EHR software development guide:
- Standardize First, Customize Later: Initial standardization of Epic implementation reduces upfront costs significantly. Epic customizations can be added incrementally as workflows stabilize.
- Proactive Training: Establish “super-user” training programs to lower ongoing training expenses, reducing recurring maintenance fees and operational inefficiencies.
- Strategic Partnerships: Collaborate with certified Epic consultants who specialize in efficient deployments—reducing long-term support and upgrade costs.
KPI to Watch:
Organizations using targeted, upfront standardization and training best practices report a 25–30% reduction in hidden costs within the first two years post-deployment.
Long-Term Benefits of Epic EHR for Healthcare: Planning for Sustainable Success
Epic’s initial price tag is daunting, but the Epic electronic health record cost must be evaluated against substantial long-term benefits—far beyond immediate operational efficiencies. Strategically, Epic positions healthcare organizations for sustained competitive advantage.
- Operational Excellence: Epic consistently reduces overall operating costs by integrating financial, clinical, and administrative data into one cohesive platform, reducing redundancies significantly.
- Regular Upgrades & Innovation: Included in your subscription or license fees are ongoing enhancements that improve patient care and maintain compliance with regulatory requirements.
- Patient Engagement & Satisfaction: Epic’s integrated patient portals and communication platforms improve patient satisfaction scores—critical KPIs on consumer-oriented websites like Healthgrades or patient review sites, directly impacting your organization’s market position.
Practical Takeaway:
Plan financially for a 5-10 year horizon, leveraging Epic’s ongoing improvements. Healthcare leaders report seeing tangible operational benefits within the first three years, with deeper ROI realized beyond year five.
How Topflight Keeps Epic Projects on Budget —and on the Marketplace
Epic roll-outs spiral past forecasts when every workflow tweak means bespoke code, a fresh HIPAA review, and another pass through App Orchard gatekeepers. We shortcut the pain: our engineers have already shipped Epic-connected apps that stream wearables (RTHM), drive computer-vision rehab (Allheartz), and sailed through Connection Hub on the first submission. These wins didn’t just save calendar time—they helped clients lock in $188 million+ in follow-on funding, proof that disciplined budgets and investor traction go hand-in-hand.
And we don’t stop at integration. From launch analytics that surface ROI for CFOs to optimization sprints that trim per-patient licensing costs, Topflight turns Epic into a growth lever instead of a cost center.
Why teams pick Topflight for Epic EHR integration
-
App Orchard / Connection Hub muscle – Sandbox setup, OAuth creds, pixel-perfect review: we handle the red tape so your listing goes live minus déjà-vu resubmissions.
-
Cost-controlled sprints – Pre-vetted SMART on FHIR connectors and reusable UI blocks shave weeks off dev time (and six figures off burn).
-
Compliance baked in – HIPAA, SOC-2, and PKCE from sprint one; no last-minute “security tax.”
-
Investor-proven ROI – Apps we’ve built help founders close nine-figure rounds—evidence your board will actually care about.
Ready to make Epic behave like your product—without torching the budget? Let’s talk.
Is Epic EHR Worth the Investment in 2026?
By now, it’s clear: Epic EHR is a significant financial decision that can redefine your healthcare organization’s operational landscape—but only if approached strategically. Its enterprise-grade capabilities, deep integrations, and advanced AI-driven workflows offer exceptional value for money, provided you’re ready for the substantial upfront investment. But let’s revisit the essential question decision-makers often ask: how much does Epic EMR cost in reality?
Given Epic’s sizable financial commitment, it’s critical to develop a clear, detailed plan that aligns closely with your organizational goals, size, and long-term objectives. For many healthcare leaders, the measurable improvements in patient outcomes, clinician productivity, and streamlined workflows justify Epic’s premium pricing—assuming thoughtful deployment, rigorous budgeting, and strategic integration are part of your roadmap.
Bottom line: If your organization’s scale and operational complexity justify Epic’s high costs, and you’re strategic about managing hidden fees, Epic remains a strong contender to drive substantial healthcare improvements and long-term returns.
Frequently Asked Questions
Can smaller clinics realistically afford EPIC EHR?
Standalone small clinics usually struggle with Epic’s high upfront costs. However, joining larger community-hosted Epic systems or consortiums can significantly lower expenses, making Epic more financially viable for smaller providers.
How long does an average EPIC implementation take?
For large hospitals, expect 18-24 months from planning to go-live. Smaller clinics typically see timelines closer to 6-12 months, depending heavily on customization and data migration complexity.
How often does EPIC update its software, and does this incur additional costs?
Epic typically rolls out updates quarterly. While minor updates are covered by annual fees, significant upgrades or custom enhancements can involve additional service charges—so always budget accordingly.
What's the typical timeframe to achieve ROI from EPIC implementation?
Most organizations see initial operational improvements within 1–2 years, but significant ROI typically materializes 3–5 years post-deployment, once adoption stabilizes and workflows become optimized.
Can we migrate data ourselves to reduce EPIC EHR implementation costs?
Self-managed migrations can save money initially but often lead to data errors and workflow disruptions. Professional EHR integration services are recommended to ensure accuracy, compliance, and smooth operations.
Does EPIC support interoperability with other EHR systems like Allscripts or Cerner?
Yes, Epic does offer integration with major EHR vendors, but custom interfaces can become costly. Budget $1,000–$5,000 per interface, and clearly define your interoperability goals to control expenses.