Switching an EHR isn’t like switching a mobile app. For a medical facility, it’s a high-friction reset: patient registration edge cases resurface, EHR users lose speed, care coordination gets noisier, and you spend real money training staff back to baseline—while still protecting patient health information.
That’s why EHR decisions are treated like core infrastructure. In KPMG’s 2025 Healthcare CEO Outlook, 75% of healthcare CEOs call electronic health records “very important” for digital transformation (another 19% say “important”). And KPMG’s warning is clear: modernization expands the attack surface, so cybersecurity must keep pace.
If you’re creating an EHR, this guide covers EHR application development end-to-end—so you can make an electronic health record system that scales safely.
Top Takeaways:
- Before attempting to build an EHR system from scratch, see how you can leverage existing software by integrating EHR data with lightweight doctor- or patient-focused front end applications.
- When working on a full-fledged EHR/EMR platform, you’ll need to create multiple applications optimized for different user roles and potentially supporting various platforms across web and mobile.
- Rapid prototyping is an essential part of EHR development and helps us align an EMR system’s features with specific healthcare providers’ goals and practices.
Table of Contents:
1. What’s the Difference Between EMR and EHR
2. Benefits of EHR Systems
3. Ready-Made vs. Custom EHR Solutions
4. Must-Have Features of a Modern EHR System
5. Types of EHR Systems
6. Complete EHR Software Development Roadmap
- Step 1: Establish a Data Migration and Interoperability Plan
- Step 2: Identify Core Modules
- Step 3: Get Key Functional Requirements
- Step 4: Ensure Compliance with Regulatory Standards
- Step 5: Design System Architecture
- Step 6: Choose Technology Stack
- Step 7: Create Custom UI/UX for Clinical Workflows
- Step 8: Integrate APIs and Third-Party Services
- Step 9: Implement Data Security, Encryption, and Backup Measures
- Step 10: Prepare for Launch
- Step 11: Execute Testing and Validate System Functionality
- Step 12: Roll Out in Phases and Train Clinical Staff
- Step 13: Provide Ongoing Support and Continuous Optimization
7. Tech Stack for Building EMR/EHR Software
8. EHR/EMR System Development Cost
9. Topflight’s EHR Development Expertise
10. Selected EHR/EMR Integration Projects
What’s the Difference Between EMR and EHR
People (including plenty of healthcare professionals) use “EMR” and “EHR” interchangeably—and honestly, a lot of EHR/EMR providers like Epic and Cerner don’t help, because they sprinkle both terms across their sites like seasoning.
Still, if you’re building software (or buying it), the distinction is useful: EMR usually describes a record that lives mainly inside one practice, while EHR implies the record is built to travel across organizations and support broader care coordination. Here’s the quick comparison:
|
Feature |
EHR (Electronic Health Record) |
EMR (Electronic Medical Record) |
|---|---|---|
|
Definition |
A digital version of a patient’s complete health record accessible by multiple healthcare providers. |
A digital record of a patient’s medical history used primarily by a single healthcare provider. |
|
Scope |
Covers a broader view of a patient’s health across different settings and providers. |
Focused on clinical history within a single practice or organization. |
|
Interoperability |
Designed to be interoperable (can share data across systems/providers). |
Limited interoperability; often stays within the facility where it was created. |
|
Data sharing |
Facilitates exchange of patient data between multiple providers and facilities. |
Data sharing is typically restricted to the organization that created the record. |
|
Purpose |
Supports continuity of care across the patient journey (multiple touchpoints). |
Supports diagnosis and treatment inside one practice’s workflow. |
|
Functionality |
Often includes wider datasets (labs, meds, immunizations, history, etc.). |
Often centers on diagnoses, treatment plans, and visit notes for that practice. |
|
Patient access |
More likely to support patient access via portals and cross-provider experiences. |
Patient access is more limited or may be unavailable. |
Why this matters for healthcare app development: if you’re building something meant to work across providers (referrals, labs, hospital + clinic handoffs, population health, multi-site networks), you’re effectively in EHR territory—interoperability expectations come with the job. If you’re optimizing one clinic’s internal workflow, you may be closer to an EMR pattern.
And yes, standards bodies like the ONC have their own definitions and nuance—but for most teams, this “scope + shareability” mental model is the only part that affects real product decisions.
So what is an EHR system, in plain English?
An Electronic Health Record (EHR) system is the digital backbone that stores, manages, and shares patient health information securely across the care team. The key word is share: an EHR is built to move with the patient—across clinics, hospitals, labs, and specialists—so healthcare professionals aren’t forced to treat every visit like a first date.
In practice, a real EHR usually bundles:
- demographics + patient registration
- problem list, allergies, meds
- visit notes, orders, and results (labs/imaging)
- care plans + care coordination
- access controls + audit trails (because data breaches are a thing)
Benefits of EHR Systems
Nobody wakes up excited to click through an EHR. But there’s no going back to handwritten charts. Even if some clinicians call modern EHR/EMR systems “glorified cash registers,” the right setup still wins on speed, safety, and coordination.
The fastest ROI usually comes from boring wins—routing, reminders, reconciliation—aka medical record automation done consistently.
One caveat before we start clapping: you don’t get these benefits by installing software. You get them when workflows are designed intentionally, staff are trained, and the system has the essential features (plus an intuitive interface) people can actually use.
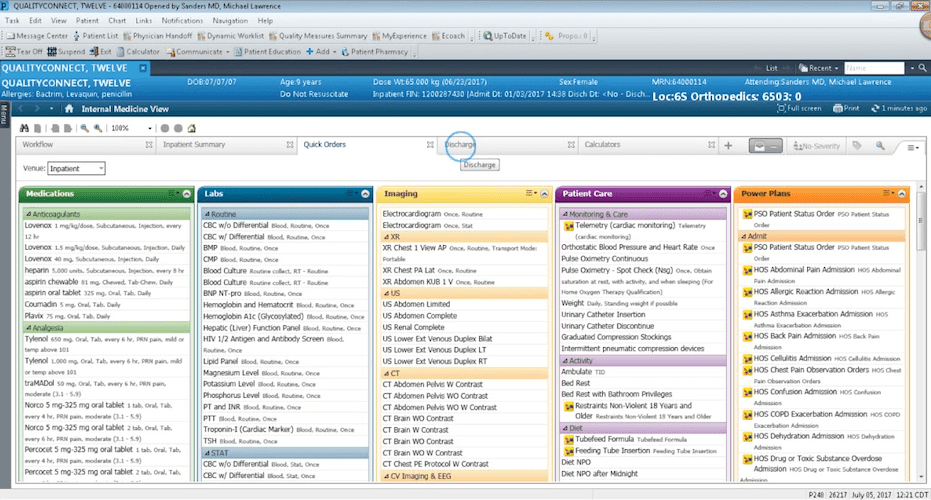
Some doctors still have to suffer through this (in our day and age!)
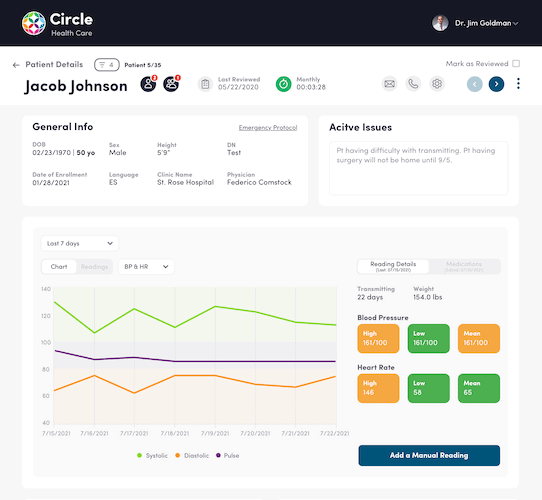
1) Increased Efficiency (less busywork, fewer bottlenecks)
Automation in EHR software can streamline internal workflows in a healthcare facility—when it’s configured for how clinicians work (not how vendors demo).
- faster decision-making (less chart-hunting)
- fewer manual handoffs and duplicate admin tasks
- less overtime spent on documentation clean-up
- better morale because the system stops fighting the staff
2) Better Patient Outcomes (more care time, less screen time)
When clinicians aren’t trapped in a maze of clicks, they can focus on patients.
- more consistent follow-ups and continuity of care
- fewer errors caused by missing context and poor data accuracy
- stronger patient–physician relationships
- lower avoidable readmissions (when discharge + follow-up workflows are supported)
3) Optimized Costs (stop paying for preventable waste)
EHRs don’t magically “save billions,” but they can reduce leakage across clinical and administrative workflows.
- fewer duplicate tests and avoidable rework
- fewer revenue-cycle misses from incomplete documentation
- better throughput and capacity planning from cleaner operational data
4) Better Coordination (the benefit people feel first)
Care coordination is where an EHR either shines—or fails loudly. A good system keeps the care team aligned.
- smoother handoffs across departments and external providers
- fewer “fax it to me” moments and missing-history surprises
- everyone working from the same problem list and plan
5) Stronger Security + Regulatory Compliance (because reality bites)
Centralizing patient data raises the stakes. The upside: EHR platforms can enforce consistent controls—if you actually configure them.
- role-based access, audit trails, and safer defaults
- data encryption (in transit and at rest) as a baseline, not a “nice-to-have”
- fewer compliance fire drills because records, access logs, and workflows are standardized
6) Better Decisions + Patient Engagement (turn records into signals)
Once data is structured, EHR software becomes more than storage—it becomes a decision support layer.
- reporting and analytics to spot bottlenecks and quality gaps
- proactive outreach (e.g., missed follow-ups, chronic care reminders)
- portals and self-service that reduce phone tag and keep patients in the loop
This is the “why” behind EHR/EMR systems. Next, let’s get practical: what you’re actually building—and which features matter first.
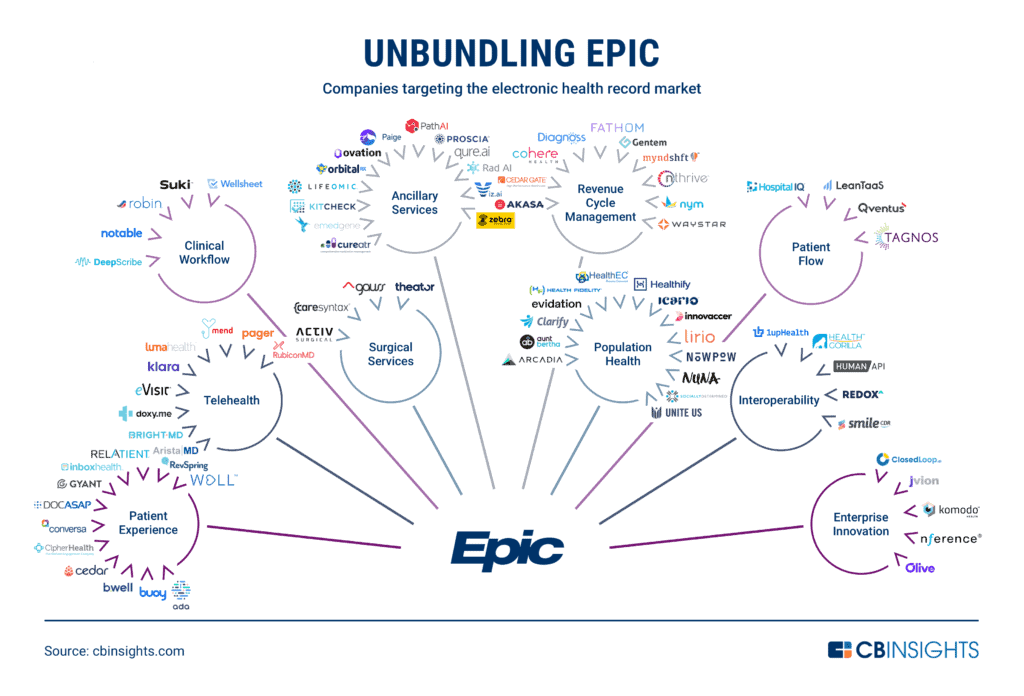
Ready-Made vs. Custom EHR Solutions
When we talk about software, there are really only two options of handling it — either you adopt software or the software adopts you. If you’re still in vendor land, this checklist helps you avoid picking a shiny demo over a workable reality: choosing an EHR system.
The seemingly easier route is to go and implement one of the well-known EHR systems, such as Epic, Cerner, Allscripts, you name it – instead of custom EMR/EHR software development. Such an approach has its advantages and drawbacks:
Implementing an Out-of-the-Box EHR System
| Pros | Cons |
|
|
As you can see, this is the scenario where software adopts you. You need to learn how to use it, find a way around its quirkiness and integrate it with everything else you’re using, train personnel, etc.
Alternatively, you can build your own EHR platform, and it doesn’t have to be that scary hairy thing from the 90s. If we like working with Gmail or Facebook, why can’t we create EHR software that works and feels as intuitive?
Related: How to integrate your health app with EPIC EHR/EMR and Allscripts EHR integration.
The flashforward is we can, but we’ll talk about that later. For now, let’s see what the implications are with custom EHR software development
Developing a Custom EHR System
| Pros | Cons |
|
|
Opting for EHR custom software development allows healthcare providers to tailor their system to meet specific needs, from patient record management to clinical decision support. This customized approach is a major advantage over out-of-the-box solutions, which often lack the flexibility required by different medical practices.
For a more detailed breakdown of the EHR cost, you can visit our comprehensive guide on EHR implementation.
Must-Have Features of a Modern EHR System
Clinical Documentation Module Development
-
Scope: SOAP/APS/OCT notes, reusable templates, smart phrases, structured fields (SNOMED CT, LOINC), ICD-10 capture, vitals.
-
Builder notes: Offline-first edits, autosave, versioning, merge/conflict resolution for concurrent edits, e-sign, full audit trail; insert points for CDS Hooks.
-
Interop model: FHIR Encounter, Observation, Condition, Procedure, Composition/DocumentReference; align to USCDI.
-
Guardrails: Field-level permissions, “break-the-glass,” minimum-necessary views, PHI redaction for analytics exports.
-
Ops KPIs: Note-closure time, coding accuracy, template reuse rate, addendum frequency.
-
Gotchas: Free-text bloat, template rot, copy-forward risks, duplicate Observations across apps.
E-Prescribing System Integration
-
Capabilities: New/change/cancel Rx, refills, eligibility/formulary checks, interaction/allergy screening, prior auth, EPCS (DEA 2-factor), pharmacy directory sync.
-
Standards: NCPDP SCRIPT; RxNorm/NDC; FHIR MedicationRequest, Medication, MedicationStatement.
-
Compliance: Identity proofing for prescribers, EPCS token management, immutable audit, clock drift checks on 2FA.
-
Ops KPIs: eRx success rate, renewal turnaround time, hard-stop override rate.
-
Gotchas: State-specific eRx mandates, test→prod cutover quirks, cancellation flows missed in QA, DEA audit readiness.
Laboratory Information System Integration
-
Capabilities: Order entry (panels), specimen labeling, results ingestion, abnormal flag routing, delta comparisons, attachments (PDF/DICOM refs), send-out tracking.
-
Standards: HL7 v2 (OML/ORU), LOINC mapping; FHIR ServiceRequest, DiagnosticReport, Observation.
-
Workflow: Result reconciliation with provider acknowledgment and patient notification rules.
-
Ops KPIs: Result turnaround time, unmatched result rate, abnormal acknowledgment SLA.
-
Gotchas: LOINC drift across labs, one-off compendium codes, multi-lab normalization.
Revenue Cycle Management Components
-
Capabilities: Charge capture, coding assist (ICD-10-CM, CPT/HCPCS), claims (837), ERA posting (835), denials management, real-time eligibility (270/271).
-
Standards/Data: FHIR Coverage, Claim, ClaimResponse, ExplanationOfBenefit.
-
Controls: Segregation of duties, PHI tokenization for exports, payer-rule cache with versioning.
-
Ops KPIs: First-pass acceptance %, days-in-AR, denial rate, clean-claim velocity.
-
Gotchas: Clearinghouse edge cases, missing superbills from quick visits, payer-specific bundling rules.
Patient Portal & Messaging
-
Capabilities: Appointments, results, secure messaging, intake/e-consent, telehealth join, payments, proxy access (pediatrics/elder care).
-
Standards: SMART on FHIR/OAuth2; FHIR Patient Access APIs; align disclosures to USCDI.
-
Safety: MFA, session limits, message retention policies, teen privacy flags, minimum-necessary threading for staff.
-
Ops KPIs: Portal activation %, message SLA, no-show reduction, intake completion rate.
-
Gotchas: Identity proofing, duplicate patient accounts, untriaged inbox overload, “right of access” conflicts with clinical judgment.
Clinical Decision Support & Quality Reporting
-
Capabilities: Rules engine for alerts/ordersets/care gaps, registries, measure tracking (MIPS, HEDIS, eCQMs), care plans.
-
Standards: CDS Hooks, CQL, FHIR Measure/MeasureReport, PlanDefinition, Library.
-
Governance: Tiered alert severity, fatigue monitoring, post-deployment review loops, change management for rules.
-
Ops KPIs: Alert acceptance rate, override reasons, measure pass rates, documented gap closures.
-
Gotchas: Stale rules, version chaos across environments, “global” measures that miss specialty nuance.
In practice, AI in EHR automation can extend these capabilities with predictive insights, note summarization, and workflow automation.
Types of EHR Systems
Primary Care EHR Development
Primary care lives and dies on panel management: chronic disease follow-up, preventive care gaps, and fast refills without melting the inbox. Your EHR should make a 15-minute visit feel like 20 by front-loading context (last A1C, BP trend, care gaps) and giving clinicians one place to order, document, and message.
-
Design for flow: single-screen vitals→assessment→orders; templated chronic-care notes that auto-pull recent Observations.
-
Close care gaps: registry views + eCQM dashboards; care plans tied to tasks, not PDFs.
-
Right boundaries: FHIR at the API edge (USCDI), internal domain models inside; eRx with EPCS where needed.
-
Inbox sanity: triage rules and quick-actions for renewals; proxy access policies for families.
Watch out: overstuffed templates and free-text creep will nuke your quality reporting and burn minutes you don’t have.
Specialty Practice EHR Systems
Specialists don’t want “primary-care-plus.” They need precision: laterality in ortho, regimen tracking in oncology, trimester context in OB, validated screeners in behavioral health. Start by mapping the true clinical artifacts (flowsheets, calculators, imaging priors) and only then design notes and ordersets around them.
Make the imaging loop first-class: order routing, PACS viewer, priors side-by-side, and structured impressions mapped to LOINC/SNOMED. For behavioral health and SUD, plan for data segmentation and consent at the field or section level—not as an afterthought.
Checklist
-
Purpose-built flowsheets with decision support at order time (CDS Hooks), not post-hoc alerts.
-
Exact coding semantics (laterality, staging, devices) to avoid “miscoded but documented” outcomes.
-
Segmentation controls for sensitive notes/results and narrow sharing scopes.
Pitfall: forcing generic templates onto specialists guarantees junk data and alert fatigue.
Hospital EHR Implementation
Hospitals are interface factories. You need bulletproof ADT, orders/results that never get “stuck,” and closed-loop meds that keep patients safe during outages and shift changes. Think of the build as three planes you must land together: clinical, operational, and identity.
-
Core plumbing: HL7 v2 (ADT/ORM/ORU) for systems of record; C-CDA for document exchange; FHIR R4 for APIs/SMART apps.
-
Identity & access: SSO (SAML/OIDC), patient identity via IHE PIX/PDQ, and “break-glass” with reason + immutable audit.
-
Safety ops: downtime/read-only modes, barcode MAR, escalation rules for critical results and device alarms.
-
Reporting: eCQMs and service-line dashboards built on PHI-aware data marts, not CSVs in email.
Pitfall: wiring interfaces before governance and runbooks—your first 2 AM outage will become a safety event.
Ambulatory EHR Solutions
Ambulatory is throughput and cashflow: tight scheduling, clean claims, fast telehealth joins, and a portal that actually reduces calls. Design around visit velocity—self-check-in, eligibility checks before the rooming starts, and note templates that don’t require a scavenger hunt.
-
Scheduling that behaves: FHIR Schedule/Slot/Appointment, templated provider calendars, and no-show reduction via reminders + portal.
-
Lean RCM: real-time eligibility (270/271), estimates at check-in, 837/835 clean-claim loops, and denial feedback into templates.
-
Patient experience: secure messaging, e-consent/intake, proxy access; SMART on FHIR add-ons for niche workflows.
-
Ops analytics: cycle time, show rate, first-pass acceptance—review weekly, adjust templates monthly.
Pitfall: untriaged inboxes and ad-hoc scheduling rules will drown staff; set triage protocols and guardrails early.
Complete EHR Software Development Roadmap: Step by Step
As you can see, it’s not exactly rocket science — EMR software development pays off in huge dividends in the long run. I suggest we jump right into action and start discussing how to build an EHR system. After all, isn’t this why you’re here?
Once you’ve skimmed through the steps below, the question “How to create an electronic medical record system?” will no longer sound daunting at all.
To guide you through the process step by step, here’s an overview table of the key phases involved in how to build an EHR system, breaking down each stage for clarity and focus.
| Step | Description |
|---|---|
| Step 1: Get Data Migration Plan | Prepare your EHR system to import legacy data accurately and communicate with external systems via standards like FHIR and HL7. |
| Step 2: Identify Core Modules | Define essential modules like patient records, scheduling, billing, and eRx. Prioritize MVP features to avoid overengineering. |
| Step 3: Get Key Requirements | Gather and validate user-specific requirements to guide development and ensure alignment with real clinical and administrative workflows. |
| Step 4: Ensure Compliance | Address HIPAA, SOC 2, ONC certification, and other regulations early to avoid costly rework later. |
| Step 5: Design System Architecture | Plan the data flow, backend services, and security layers. Align UI and core feature architecture with agile best practices. |
| Step 6: Choose Technology Stack | Select backend, frontend, and database technologies that align with your team’s expertise, scalability goals, and compliance needs. |
| Step 7: Create Custom UI/UX | Build user-centered designs based on actual workflows. Prototype, test, and refine with real clinical users. |
| Step 8: Integrate APIs, etc. | Add connectivity to labs, pharmacies, telehealth, and wearable data using secure APIs and an event-driven architecture. |
| Step 9: Implement Data Security | Apply HIPAA-compliant encryption, access control, and automated backup strategies to protect patient data. |
| Step 10: Prepare for Launch | Finalize documentation, perform readiness checks, and coordinate your team for a smooth go-live experience. |
| Step 11: Testing and Validation | Run functional, load, and security tests. Simulate edge cases and validate performance in real-world clinical environments. |
| Step 12: Phased Roll-Out/Train Staff | Deploy the system gradually and tailor training by user role to ensure adoption and minimize disruption. |
| Step 13: Support and Maintenance | Monitor feedback, ship regular updates, and maintain compliance to keep the EHR system aligned with evolving needs. |
Now, let’s dive in into this complete EHR development roadmap.
Step 1: Establish a Data Migration and Interoperability Plan
A robust data migration and interoperability plan is one of the first things that should be tackled in your EHR journey—not tacked on later. This step is not just about “importing legacy data.” It’s about ensuring your new EHR can both absorb data from previous systems and communicate with other platforms in the healthcare ecosystem.
That includes planning for:
- Legacy data formatting, cleanup, and validation
- Mapping historical records to new data models
- Choosing interoperability protocols (e.g., FHIR, HL7)
- Establishing connections to labs, imaging systems, pharmacies, and even health information exchanges (HIEs)
Don’t forget: even if you build a great EHR, it won’t be adopted if it can’t talk to the systems your partners and clinicians already rely on.
Data migration
Migrating existing patient records into a new system is a foundational step in building EHR software. The process must preserve every detail to maintain continuity of care and regulatory compliance (e.g., HIPAA, audit trails, data retention policies).
You probably already keep patient data in a system of sorts. Therefore, migrating that data into the EHR without losing any information is vital for ERM software development. Other data practices include caching.
For example, it’s recommended to cache data on mobile to not lose data and sync it correctly. Imagine a doctor entering patient information while being offline; then, when the device comes online again, the software needs not only to upload the missing data but also sync back from the EHR anything other team members might have entered in the interim – all of that without overwriting or losing any info.
APIs
API integration is essential in developing an interoperable EHR system, allowing seamless data exchange with labs, pharmacies, and third-party services. This ensures your platform supports clinical workflows and real-time access to patient data.
APIs ensure EMR interoperability: being able to send and receive data (e.g., lab results) in prerequisite formats, process it, and then output for customers on the respective platform. That’s where FHIR by HL7 and other data standards and coding (e.g., CPT, DICOM, CCD) come into play.
With Specode’s AI-powered capabilities, custom healthcare software development for EHR/EMR systems becomes incredibly fast and flexible, allowing for seamless integration and unmatched performance.
APIs play a critical role in enabling EHR custom software development by allowing systems to pull patient visit data, manage medication lists, and synchronize treatment plans across multiple platforms seamlessly.
Step 2: Identify Core Modules
Before diving into design or development of an EHR system, you need to map out the core modules your EHR system will include. Think of this step as drawing the first real outline of your product — identifying what needs to exist from day one versus what can wait. These modules aren’t just features; they’re the backbone of your clinical and administrative workflows.
Some of the most common modules to consider:
- Patient records and charting
- Appointment scheduling
- Lab and imaging integration
- Billing and insurance handling
- E-prescriptions
- Communication tools (internal chat, patient messaging)
- Reporting and analytics
- Role-based access control
You won’t need them all upfront — which is why identifying the initial core is so critical. This connects directly to your MVP strategy.
See Must-Have Features of a Modern EHR System for the deep-dive.
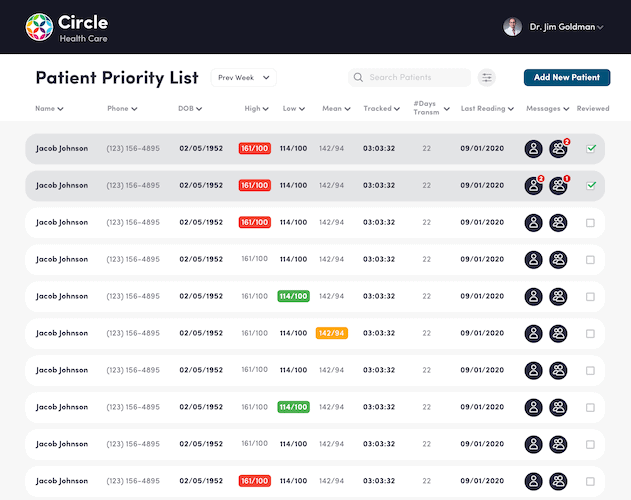
Realize you’ll be building more than a single app
Successful EHR system development often involves building a suite of apps—patient portals, clinician dashboards, admin panels—not just one interface. Each must support unique workflows and secure data access.
If you think of it, that’s really hard to miss. Yet, most companies talking about EHR development skip the part where they tell you you’ll be building multiple apps.
That’s something you can’t escape realizing during the strategy workshop. Because going through your target audience’s needs, you can’t help but notice that a lot of people will be using your EHR system in a lot of different ways.
You can think of nurses and doctors filling in patient details or looking up their vitals and other info on the platform. Then there will be front-office workers, administrators, and management using the system, right? They will use it on different devices.
Therefore, the question becomes, “How do we fit all of that into a single EHR platform?” How do we create EMR software that works equally well for all users on smartphones, desktop machines, tablets, etc.?
- multiple front-ends (that’s how developers call apps we, users, interact with)
- APIs layer
- security mechanisms
- back end with databases
Related: Complete Guide to Building a Healthcare App
That’s a very simplistic illustration of what a typical EHR platform would look like. However, the bottom line is that you and your team will be working on several separate applications. Let’s say:
- a tablet-optimized application for doctors
- a smartphone and a web-based (works best in desktop browsers) apps for doctors
- a web application for administration and management
As you already know, when you build your own EHR software, nothing stops you from building independent applications (that still work in tandem, syncing all clinical data) for different user roles based on their unique needs.
Minimal viable product is your everything
When creating EHR software, a tightly scoped MVP helps you stay lean while validating the most critical features—like patient charts, scheduling, or lab results—in real healthcare environments.
Even though a clinic, private practice, or hospital may benefit from implementing all possible applications that make up an EHR system, you need to focus on your ROI goals.
What parts of the system are likely to produce an immediate payback? Which parts of your healthcare system will benefit most from EHR automation? Start with them. There’s no need to start EHR/EMR software in its entirety, with all possible bells and whistles.
Related: MVP App Development: Everything You Need to Know
In my opinion, the ideal scenario would be, to begin with a single app for doctors and nurses (which will adapt its interface based on a user role) and another one for admins. Even then, you should trim features to the bare minimum that will drive measurable value, for example:
- faster test results from labs
- built-in e-prescribing
- on-the-go patient’s health medical history
Once the metrics are confirmed, you will continue improving on your minimal viable product (MVP), drawing funds from lowered expenses or new revenue streams. Use a minimum viable product healthcare approach first—ship the smallest workflow that proves real clinical value, then iterate once you’ve seen what users actually do (not what they say they’ll do).
This MVP thing and your decision about which parts of the EHR system to start with naturally belong to the strategy step.
Step 3: Get Key Functional Requirements
Nailing down functional requirements is critical before you develop EHR software. You’ll define how the system supports patient care, clinical documentation, compliance reporting, and more—long before any coding begins. You need a sharp, reality-checked understanding of what your EHR must do — for whom, and why. This step sets the foundation for every design and engineering decision downstream.
Think of it in three parts:
Assessment
Start by exploring your current pain points. What workflows are inefficient? Where do you lose time or data fidelity? What are clinicians, admins, and patients currently complaining about?
Scope Definition
Once the gaps are clear, you’ll need to define which features are mission-critical versus nice-to-have. This also includes setting boundaries — what won’t your EHR do in v1?
Business Case
Tie your functional needs back to measurable outcomes. Are you reducing readmission rates? Improving billing accuracy? Shortening appointment cycles? These anchor your MVP and long-term roadmap in ROI logic, not wishlist thinking.
This is not just a list-making exercise. It’s about aligning your product vision with clinical reality and financial viability.
No surprise here. Any project, be it EHR system development or clinic construction, requires thorough research and planning. You’ll have to answer questions like:
- Who will be the primary users of this new EMR system?
- What is the end goal for implementing an EHR?
- Do I have some target dates for delivering the system?
- How will I measure the success of the project?
These and myriad other questions will need answers to shape the project scope accordingly. Ultimately, the deliverables of the strategy session will come down to:
- lean canvas (just a clever word for business plan/model)
- high-level, prioritized feature list
- approximate diagram of the EHR’s architecture
When planning EHR system design, it’s crucial to align the system with the workflows of your healthcare organization. Consider the various roles that will interact with the system—whether you’re looking to create an EMR system or build a comprehensive EHR platform. Each role, from administrative staff to doctors, will require different functionalities.
Most development agencies love when a customer comes with a ready plan and a clear vision, so they can start executing without delay. Others, like Topflight, prefer to help you form your strategy, sometimes starting with nothing but a napkin sketch.
For example, we’d take you through a well-defined discovery process and help you align your EHR vision with your end goals tied to specific ROI metrics.
Related: How to Build a Medical Startup
Step 4: Ensure Compliance with Regulatory Standards
In creating a HIPAA-compliant EHR system, regulatory alignment isn’t optional—it’s baked into every feature from user authentication to audit logs. Certifications and privacy protocols should be validated early, not patched on later.
For U.S.-based products, HIPAA compliance is non-negotiable. But depending on your scope, you might also need to meet:
- HITECH regulations
- ONC-ATCB certification for meaningful use
- CE Marking (if entering the EU market)
- SOC 2 or ISO 27001 (for enterprise partnerships)
This step isn’t about checking a box. It’s about baking compliance into your product architecture, access policies, and operational workflows from the ground up.
Security and HIPAA compliance
Of course, as any healthcare solution dealing with protected health information (PHI), EHR software must comply with HIPAA regulations.
We covered the topic ad nauseam in separate blogs, e.g., here: Comprehensive Guide HIPAA-Compliant Application Development.
Among other things, to make EHR software HIPAA compliant, we need to restrict access control to patient data based on user roles, and also keep automated logs running to record every action on the system for audit purposes.
Ensuring patient privacy is a cornerstone of EHR system design, particularly when handling sensitive information like allergies, disease history, and ongoing treatment records.
When you create an EHR platform, integrating certification standards such as ONC-ATCB or CE Marking ensures that your system meets the necessary regulations for safety and performance.
These certifications not only instill confidence in healthcare providers but also help streamline the approval process when rolling out new features like e-prescriptions, lab integrations, or clinical decision support tools.
Step 5: Design System Architecture
Designing the architecture of your EHR system is where the real foundations are laid—both in terms of the visual structure users will interact with and the invisible data infrastructure that makes everything run smoothly. This phase defines how core features connect, how data flows, and how to ensure the system is scalable, secure, and maintainable in the long run.
Core features: UX meets system logic
When designing an EHR system, one thing you might miss is to check with programmers whether the design is not too complex to develop. They call it technical UX validation.
Developers can offer legit shortcuts when they know a more optimal way for realizing certain features.
Of course, virtually any design can be coded into the app. However, we’re looking for an adequate blend of functionality, UI, and required effort.
Note how many EHRs have too much on-screen stuff: checkboxes, fields, tabs, menus, etc. Get more than seven major interactive elements on a single screen, and your customer is lost. This happens when software developers and designers don’t really put themselves in their client’s shoes for every specific user role.
During the design phase, it’s vital to focus on EMR software design principles that cater to both front-end users like doctors and back-end functionalities such as scheduling, reporting, and privacy management. By ensuring that your EHR and EMR software development processes incorporate user-friendly interfaces, you’ll reduce the learning curve for medical staff.
Data architecture: blueprint for information flow
Your EHR software development must include a robust data architecture that supports secure storage, HIPAA compliance, and interoperability with external systems like labs, payers, and health information exchanges.
Your system’s data architecture involves designing how patient data will be stored, queried, and synchronized across modules like appointments, billing, prescriptions, and clinical notes. Whether you’re using a relational database (e.g., PostgreSQL) or document-based storage (e.g., MongoDB), ensure it’s built to support regulatory requirements like HIPAA audit logging and role-based access.
Plan for real-time data sync between front-end clients and backend services—especially if your EHR system will support offline mode or distributed clinical environments. Also, consider future integrations with FHIR-based systems and national networks from day one.
Aligning architecture with agile
The design stage really kicks in the agile development cycle. Without boring you to death, the agile methodology is the golden standard in the software development industry.
Related: Agile App Development: Building Winning Products
Agile means there will be several iterations for the design and all consecutive steps of the EHR development process. Even after the release, because great products tend to grow, reflecting the market dynamics and changing user needs.
Therefore, the agile approach helps establish the necessary processes, team composition, tools, and everything required to sustain an EHR long term.
Step 6: Choose Technology Stack
Choosing the right technology stack for your EHR system is not just a technical decision—it directly affects your app’s speed, reliability, regulatory readiness, and even time-to-market. The right stack ensures that your developers can build, scale, and maintain the app without running into constant bottlenecks.
Aligning stack with team composition
When developing custom EHR software, your tech stack must align with your team’s capabilities—whether it’s React for front-end, Node.js for APIs, or PostgreSQL for patient data. Don’t choose tools your team can’t master.
Needless to say, you need to work with a team having plenty of experience building EHR solutions. If you are building an EHR from scratch, the following team composition should suffice:
- front-end devs (iOS/Android/React, etc. — based on the apps you’re building)
- full-stack back-end developer for working on the core logic, database, security, etc.
- dedicated API developer
- QA engineers
- UX/UI designer
- Product manager
- Project manager
You may be surprised to see two seemingly similar roles like product and project manager on the list. However, those are pretty different. While the product manager ensures your vision is carefully carried over to healthcare app developers, the project manager is busy with handling development, design, and testing tasks day-to-day.
Your tech stack choices should reflect the skills of your team and the specific requirements of the EHR product. For example:
- Front-end: React (web), React Native or Flutter (mobile) to enable cross-platform speed.
- Back-end: Node.js, Django, or .NET depending on performance, scalability, and HIPAA compliance features.
- Database: PostgreSQL or MongoDB for structured vs. flexible schemas, depending on how your clinical data is modeled.
- APIs: REST or GraphQL for modern, interoperable interfaces. FHIR compatibility is a must for EHRs that plan to integrate externally.
Cloud platforms like AWS, Google Cloud, or Azure offer HIPAA-ready environments with baked-in compliance tools. If you’re pursuing AI features, consider adding GPU-ready infrastructure and frameworks like TensorFlow or PyTorch to your stack early on.
Support for emerging technologies
Advanced EHR platform development increasingly includes AI, wearables, and real-time alerts. Whether parsing vitals or enabling telehealth, emerging tech is shaping how modern EHRs support patient care.
If you have a medical background, you know pretty well what features development you need in an EMR, such as patient records, charting, reports, etc. My bet is if you’re looking to build an EHR, you don’t just need electronic health records with a super user-friendly interface. You’re likely looking for more advanced features backed by the latest technologies, for example:
- AI and machine learning, helping with parsing medical data, diagnosing, and focusing doctors’ attention on patients in a risk group
- Internet of Things and wearables to feed EHR with patients’ vitals in real-time
- Telemedicine integrations
- Blockchain-based EHR for trustless operations among a consortium of companies
Related: IoT App Development Guide and Blockchain in the Healthcare
Also Read: How to Build a Wearable App for iOS and Android
Developers must also consider key integrations, such as e-prescriptions and lab tests, to streamline workflows. Additionally, building features like chat functionality for inter-staff communication or adding mental health tracking can further enhance the system’s utility for diverse healthcare settings.
It’s high time for improving providers’ EHR experience with tools like ambient scribes, automatic handwriting recognition, and AI-based imagery analysis.
Step 7: Create Custom UI/UX for Clinical Workflows
User interface design isn’t just about making things look nice—it’s about eliminating friction in clinical workflows. When done right, great UI/UX becomes invisible. When done poorly, it becomes the thing your clinicians complain about most.
Prototyping and design
UI and UX design play a vital role in custom EHR software development, helping reduce clinician fatigue and streamline patient data access. Legacy systems often suffer from bloated UIs and poor usability.
Why do doctors and nurses constantly complain about EHR systems? Why do they call them 800-pound gorillas in the healthcare industry and scold them for their click-to-death nature? Because some of them serve the healthcare system as a whole (read billing) and don’t care that much about med personnel’s needs.
Related: The Ultimate Guide to UI/UX Design and Healthcare App Design
Custom EMR development, in that sense, sets you completely free. You may design unique front ends for different users so that ERM software doesn’t get in their way.
From user flows to prototypes
Designers review the needs of your target audience and define user journeys on flowcharts to understand the most optimal way for customers to navigate around the software.
Low-fidelity designs
They then come up with rough mockups, also known as low-fidelity wireframes. It’s like sketching application screens on a napkin. Only they do that in special programs like Figma.
Figma, which we also prefer, is so popular because it allows UX/UI engineers to interconnect all designed screens. As a result, the screens come to life and react to different gestures and clicks. This effectively turns otherwise static screens into an interactive prototype.
Lately, however, our team goes straight from design to code using Figma built-in tools. We now also prefer rapid coded prototypes whenever applicable.
High-fidelity designs
The next thing on the list is to turn the primitive prototype into a high-fidelity one. That simply means updating the graphics to what users will actually see in the app. Why not start with the refined version of UX/UI in the first place? Because it’s easier and cheaper to iterate on rough wireframes.
Validate with clinical users, not just stakeholders
The sole purpose of the interactive prototype is design validation. We need to test it with users before starting development. We need to make sure that the EHR software we’re building is intuitive and fulfills customer needs appropriately. You see, programming these interfaces would take way more time than several iterations of design and user testing.
We use such tools as usertesting.com to gather feedback and improve the prototype before building EHR software.
It’s essential to test prototypes not just with product stakeholders, but with real clinical users—doctors, nurses, administrative staff—who will use the tool daily. Their insights reveal bottlenecks that aren’t always obvious in planning meetings.
Step 8: Integrate APIs and Third-Party Services
No modern EHR is an island. From e-prescriptions to lab reports, telehealth, and patient intake forms—your system needs to plug into an ecosystem of services already used across healthcare settings. The ability to integrate cleanly, securely, and reliably often makes or breaks real-world adoption.
Build for extensibility from the start
A solid EHR architecture should be API-first, which means all your system’s core functionalities—from patient record retrieval to appointment booking—should be available through documented endpoints. This makes it easier to layer on features or connect to services down the line without costly rewrites.
You’ll also want to support modern data exchange standards like FHIR (Fast Healthcare Interoperability Resources) and HL7, especially if you’re integrating with national networks or providers who demand compatibility with existing clinical systems.
Common third-party integrations
To build a fully connected EHR system, integrate essential third-party services like Surescripts for eRx, Twilio for telehealth, and lab providers for diagnostics. This improves care delivery and administrative efficiency.
Here are some typical integrations that EHR platforms often require:
- E-prescription platforms (e.g., Surescripts)
- Lab and diagnostic systems
- Telehealth providers (e.g., Zoom for Healthcare, Twilio)
- Payment processors for billing modules
- Scheduling tools (both internal and external-facing)
- Wearable and IoT devices to feed real-time vitals
- CRM and patient engagement tools
Once you start piping reminders, outreach, and campaigns, you’ll want a clean EHR CRM integration pattern (or you’ll recreate a call center inside your EHR).
These services often offer SDKs or APIs that your EHR development team will need to integrate with, authenticate securely, and maintain over time.
Future-proofing the stack
Your EHR platform should support webhooks and real-time event triggers—critical for use cases like lab result alerts or medication adherence tracking. These features enhance the user experience and are increasingly used in real-time healthcare workflows (e.g., notifying a provider when lab results arrive or triggering alerts when patient vitals cross thresholds).
This isn’t just a technical win—it’s a user experience differentiator.
Step 9: Implement Data Security, Encryption, and Backup Measures
When developing HIPAA-compliant EHR software, security features must be baked in from day one—covering encryption, data backups, and access control. Patient trust and regulatory fines are both on the line.
Data security
Set up role-based access controls so users only see what they need. Log every action—especially around patient data. Include session timeouts, brute-force protection, and anomaly alerts to cover the basics.
Encryption
Encrypt all data in transit (TLS 1.2+) and at rest (AES-256). Use managed services from HIPAA-compliant cloud providers to handle encryption keys, logs, and access policies without reinventing the wheel.
Backups
Automate encrypted, offsite backups with clearly defined RPOs/RTOs. Run restore tests regularly. The worst time to find out your backup strategy sucks is when you need it.
Step 10: Prepare for Launch
Before launching your new EHR system, you need a controlled rollout strategy, compliance checks, and a fully briefed support team. Patient care and operational safety depend on a smooth go-live process.
Get your launch checklist in order
Make sure you’ve covered critical pre-launch checks:
- Confirm role-based access is correctly configured
- Validate all third-party integrations (eRx, labs, scheduling) are stable
- Ensure performance under expected user loads (especially during peak hours)
- Review HIPAA compliance touchpoints, including logging, backups, and data retention
Also, verify that your go-live version reflects all final content from stakeholder sign-off and that a rollback plan exists—just in case.
Timing the launch and team coordination
At some point, when the product is doing what it’s supposed to do, you will launch it publicly.
Pick a low-traffic day for go-live. Make sure your devs, QA, and product team are all on standby. Assign a designated point person to triage post-launch feedback and hotfix requests in real-time.
Launch success isn’t just about stability—it’s about creating trust with your clinical users from day one.
Step 11: Execute Testing and Validate System Functionality
Stress-testing your system is a must when building robust EHR software. QA should simulate real clinical chaos to ensure performance, accuracy, and security hold up under pressure.
Quality assurance from the start
Ok, so testing goes hand in hand with development. Every new version of the healthcare software needs to be tested before shipping it into production. Developers include automatic tests right into code. Then, there’s always a QA engineer going through all possible scenarios, trying to “break” the system from all imaginable angles.
Related: QA Guide: Steps, Tools, Best Practices and More
Go beyond basic QA during EHR development
System validation should include:
- Functional testing (do features work as expected?)
- Regression testing (did recent changes break anything?)
- Load testing (can it handle real-time usage from multiple users?)
- Security testing (is your data leak-proof under stress?)
You should also test edge cases—like poor Wi-Fi, outdated devices, or simultaneous data edits from different roles—to mimic real clinical environments.
Include clinical validation
Finally, validation must involve real end users: physicians, nurses, billing admins. Their hands-on feedback during final testing rounds will highlight workflow friction points that automated tests can’t catch.
Step 12: Roll Out in Phases and Train Clinical Staff
A phased rollout helps ensure successful EHR implementation, while targeted training improves staff adoption and should be included in your EHR implementation plan.
Go phased, not flashy
Start with a controlled group—like a single department or clinic—before scaling across the organization. This lets you validate workflows, uncover edge cases, and make adjustments without overwhelming your staff or support team.
Once the pilot proves stable, you can extend rollout site-by-site or team-by-team, gathering real-time feedback at every stage.
Don’t skip the training
Even the most intuitive UI won’t help if staff don’t understand it. Build training programs tailored to each user role—physicians, nurses, admins, billing teams. Include:
- Hands-on sessions
- Role-specific cheat sheets
- Shadowing workflows in real scenarios
Set up dedicated support channels during rollout to answer “how do I…?” questions quickly. The smoother the handoff, the faster the adoption.
Step 13: Provide Ongoing Maintenance and Support + Continuous Optimization
Post-launch, your team should continue to optimize and support the EHR software based on real user feedback. Regular updates, issue resolution, and feature improvements keep the system aligned with evolving healthcare needs.
Support and iteration
That’s not the end of the development cycle, though, as you will continue to work on new features, improvements, fixing some lingering minor issues, and keeping the EHR software up-to-date.
If “optimization” to your org means “we’ll revisit it next quarter,” steal a real playbook here: EHR Optimization
Of course, that process is way less intensive compared to the initial efforts for EHR implementation. Still, it’s something you need to consider and foresee a retainer team for handling all these tasks.
Feedback loops and product evolution
Establish ongoing feedback channels with your users—monthly surveys, quarterly check-ins, or in-app feedback tools. Clinical workflows evolve, and your EHR should too. When the pain is adoption + performance (not missing features), you’re often better off planning an EHR upgrade than a rebuild.
Assign a product owner or clinical informatics lead to translate user feedback into actionable updates. Prioritize enhancements that reduce friction, improve performance, or meet new compliance standards.
Even though coding is one of the most crucial parts of the entire EMR development process, it’s often little understood by business owners. And rightly so, developers might have an even harder time parsing through the daily healthcare routine of medical workers and management.
That’s exactly why post-launch support matters. It’s not just bug fixes—it’s translating the messy reality of care delivery into ongoing product updates that make life easier for clinicians and devs alike.
Tech Stack for Building EMR/EHR Software
I believe businesses choose companies or, rather, people when deciding on a development partner, not technologies. I mean, if you run into a Microsoft.net development shop, you’ll be stuck with their tech stack, regardless of your preferences. And it will be tough to convince them to switch to this new shiny thing you’ve read about at a random blog. But that should not be your concern, really. All technologies work just fine, in the right hands.
Related: How to choose the right tech stack for your application
A word of advice here would be to check whether the team can work with your existing solutions and other third-party services you want to integrate with. One more thing worth double-checking is to ask for a microservices-based approach to the EHR’s architecture, which should be an obvious no-brainer to any capable team.
FHIR-Based EHR Development
-
Modeling: Map clinical data to FHIR resources (Patient, Encounter, Observation, Condition, MedicationRequest, etc.) with clear profile/version strategy and validation on write.
-
Auth & app model: OAuth2/OIDC, SMART on FHIR launch (EHR→app and standalone), token scopes aligned to minimum-necessary.
-
Patterns: Native FHIR store vs. FHIR façade over internal models; eventing (subscriptions/webhooks) to de-couple modules.
-
Pitfalls: “Everything as FHIR” dogma slows ops; pick FHIR at boundaries, internal domain models inside.
Cloud vs. On-Premise EHR Architecture
-
Cloud (default): BAAs, private VPCs, KMS/HSM, regional controls, autoscaling, managed DBs; design for RTO/RPO with cross-region backups.
-
On-prem (only if required): Hardware lifecycle, patch windows, HA/DR complexity, physical security; budget for on-call + spares.
-
Hybrid: Edge devices or hospital data centers with cloud analytics; strict egress controls and audit replication.
-
Pitfalls: “Lift-and-shift” monoliths become expensive quickly; cost explodes without budgets for egress, logs, backups.
Interoperability Standards Implementation
-
Clinical: HL7 v2 (ADT/ORM/ORU), C-CDA for documents, FHIR R4 at the API edge (USCDI alignment).
-
Rx: NCPDP SCRIPT + EPCS; directory sync; cancellation/change flows tested end-to-end.
-
Billing: X12 270/271 eligibility, 837 claims, 835 ERA posting; keep a payer rules cache with versioning.
-
Quality: eCQMs/QRDA or FHIR Measure/MeasureReport to support MIPS-compliant EHR systems without bolt-ons.
-
Pitfalls: Silent version drift across partners; build contract tests against real payloads, not happy-path samples.
EHR Data Migration Strategies
-
Inventory: Source systems, tables, documents (PDF/DICOM), and code sets; decide authoritative sources per domain.
-
Mapping & QA: Deterministic mappings + exception buckets; reconcile counts and clinical “golden patients.”
-
Cutover: Dual-run window, read-only freeze plan, rollback checklist, comms to clinical ops; post-go-live defect triage.
-
Privacy: De-identify lower environments by default; PHI tokenization for analytics.
-
Pitfalls: Free-text note chaos and orphaned attachments; handle before weekend cutovers.
Security & Compliance Baseline
-
Controls: Role scopes, break-glass with reason capture, field-level permissions, immutable audit trails, key rotation, secrets mgmt, two factor authentication.
-
Processes: Vendor BAAs, incident playbooks, backup/restore drills (prove RPO/RTO), least-privilege IAM.
-
Evidence: Centralized logs, alerting on PHI access anomalies, quarterly access reviews, deploy gates for privacy checks.
Observability & Operations
-
Telemetry: Structured logs, metrics, and distributed tracing for every request touching PHI.
-
SLOs: Define SLIs (latency, error rate, message backlog) and wire alerts to on-call with runbooks.
-
Resilience: Circuit breakers, idempotent consumers, DLQs/retries for HL7/FHIR/X12 pipelines; chaos days on non-prod.
Reality check: tools matter less than execution, but if you’re evaluating a custom EHR development company, look for these patterns wired in by healthcare software architecture experts—not promised later in an “integration phase.” Note on terminology you’ll see in RFPs: phrases like “ONC-certified EHR developers” circulate, but ONC certifies products/modules, not people. What you actually want is a team that has shipped modules through ONC 2015 Cures Update testing.
EHR/EMR System Development Cost
$400,000+ for a mid-level EHR system. Up to $1,000,000 for a full-blown platform. Sounds scary? Well, depending on your needs, you may just need integrations, which often fall well within the $100K range. I’d say a decent prototype for the web (without mobile clients) should be doable in a $150K-$200Kish range.
And if you’re benchmarking build vs buy against the 800-lb gorilla, here’s a grounded breakdown of Epic EHR pricing dynamics.
Related: App Development Costs: The Complete Breakdown
Topflight’s EHR Development Expertise
As certified healthcare technology developers, Topflight helps teams scope, build, and integrate EHR/EMR integration projects without turning clinics into QA labs. We’re pragmatic builders: ship what moves clinical outcomes and revenue, document what matters, and prove it with audit trails—not slideware.
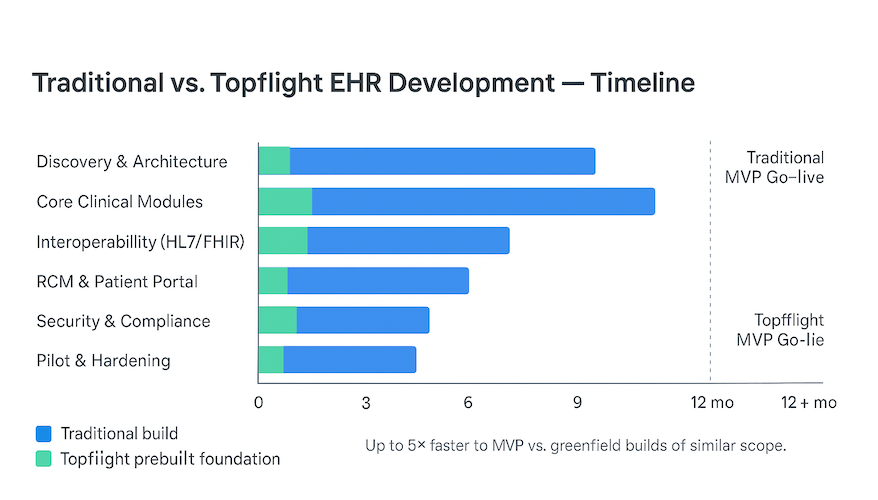
One of the options is to ship on a prebuilt EHR foundation (auth, audit, consent, documentation, patient portal, etc.). Less re-plumbing, earlier pilots, fewer integration landmines. Up to 5× faster to MVP compared to greenfield builds of similar scope (based on internal project baselines and module reuse).
-
Shared auth/audit/consent across modules → no “integration phase” to make them agree.
-
FHIR/HL7 edges standardized; internal domain models stay lean.
-
Migration playbooks (golden patients, exception buckets) reduce cutover risk.
-
Ops baked in: BAAs, immutable audit, least-privilege IAM, PHI-aware logging from day one.
I get it; most healthcare companies are interested in integration services, either looking to integrate existing EHR systems with new solutions or connecting EHRs by established vendors to some other software they use.
Check out our EHR integration services
After all, developing electronic health records from scratch almost sounds like a heroic endeavor, requiring a substantial budget and a considerable amount of time. However, EHRs don’t always have to be these humongous systems.
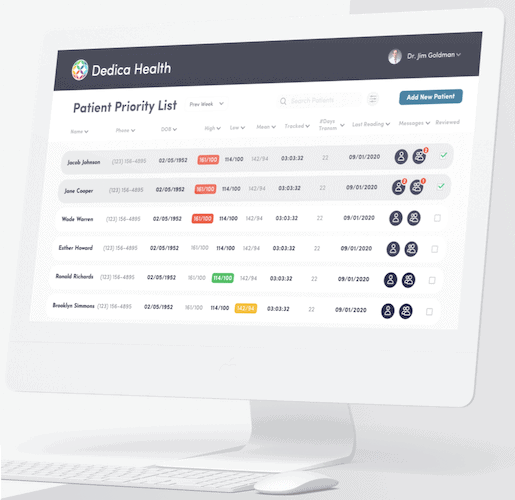
For instance, look at an RPM platform with a built-in EHR we made for Dedica. The solution is lightweight and, at the same time, very effective. Eventually, the client went on to provide the platform to other practices via a subscription model, successfully securing his first $300,000-worth ARR deal.
Selected EHR/EMR Integration Projects
#1. GaleAI — Medical Coding Accelerator (Epic & Cerner)
Cross-EHR + AI deployment with marketplace distribution: SMART on FHIR integration, FHIR compliance across targeted resources, and mini-apps packaged for both Epic and Cerner marketplaces. Mirth Connect served as the interoperability backbone where needed; we also simplified the prior-auth loop across payers and providers (pre-check + status).
Reported 97% reduction in coding time and ~15% revenue uplift from improved coding accuracy.
#2. Epic EHR integration — teleradiology workflow across facilities (NDA)
A hospital group needed radiologists to read studies remotely while keeping billing, orders, and results in sync across multiple PACS and partner sites. We implemented Epic EHR integration that tied ADT to billing, routed imaging orders to downstream systems, and posted solicited results back to Epic to close the loop.
Interfaces/standards used: HL7 v2 ADT, ORM, ORU; PACS integrations; Epic messaging to downstream systems.
#3. Epic EMR integration project — census & level-of-care dashboards (NDA)
For an operations vendor, we built an executive and care-team view of inpatient census and appropriate level-of-care, driven by Epic ADT feeds and discharge orders. DRG context and location signals improved bed-board decisions and ED-to-inpatient flow.
Interfaces/standards used: HL7 v2 ADT (demographics/service level/location), ORM (discharge orders), DRG coding.
#4. Cerner + LIMS + hospital systems — imaging & lab data in a unified app (NDA)
A non-profit chain needed a clinician dashboard that pulls imaging and lab context together. We delivered SMART on FHIR authentication with Cerner, fetched patient data from Cerner FHIR by MRN sourced from the in-house LIMS, and blended orders/results into a searchable, editable view—no writes back to Cerner by design.
Interfaces/standards used: SMART on FHIR (Cerner), FHIR R4 resources, HL7/LOINC mapping for observations, LDAP for internal SSO.
I don’t say that often, but Topflight is the right place to bring your EHR automation ideas to life. The company has intricate knowledge of what medical workers have to deal with and what can be done to help them achieve better results without burnout.
Learn more about edge computing for healthcare to explore complementary technologies that can enhance your system’s performance.
Whether you decide to make EMR or build EHR software from scratch, the result should empower your healthcare facility to offer better patient care and streamline operational efficiencies. Custom solutions allow you to integrate features like reporting, scheduling, and real-time clinical decision support, ensuring that your system evolves with your practice.
Even if you don’t have millions of dollars to invest in a brand-new EHR solution for your clinic but have secured a $100,000-$200,000 budget for IT automation, we can help you build something beautiful and engaging. Something that your staff and patients will love to use.
Related Articles:
- HIPAA Compliant App Development
- Patient Portal App Development Guide
- SMART on FHIR Appp Development
- How to build a doctor’s appointment application
- How to develop a hospital management system
- Guide to collecting healthcare data
- How to create a telehealth application
- E-Prescription App Development Guide
- EHR for Medical Billing
- Surescripts Integration: Main Steps
[This blog was originally published in January 2022, and has been updated in light of more recent information]
FAQ
What's the difference between EHR and EMR?
One uses the term “health” and the other “medical” — perfect synonyms. Some say that EMRs usually work within a single practice while EHRs work across multiple healthcare organizations. In practice, though, both EHR and EMR are used interchangeably.
Can you help us integrate third party software with our EPIC/Cerner/AllScripts EHR?
Absolutely
How long with it take to create EHR software from scratch?
12-18 months; 6-9 months for an MVP.
If there's one biggest mistake we can make with EHR development, what would that be?
Demand agile development from your development partner. You will need incremental roll-out and validation of software, which is only possible with the agile pattern.
What technology stack do you recommend for building an EHR system?
Absolutely any tech stack will work as long as you pick the right team. You shouldn’t limit yourself to specific information technology; it’s all about niche expertise and the right mix of design and development talent on a team. Probably one exception is cloud hosting: you need it, but again, that can be anything.