The COVID-19 pandemic has made telemedicine the status quo healthcare delivery model. A model that fosters doctor-patient and doctor-doctor communications via telecom technologies. In everyday life, if you can video call or chat with a doctor through a secure app without having to worry about compromising your data — you’re in the telemedicine world.
#1: Examples of telemedicine
#2: Who can practice telemedicine?
#3: What does telemedicine treat?
#4: The benefits of telemedicine and how it is bringing a quiet revolution to value-based care
#5: Enabling remote care with mHealth
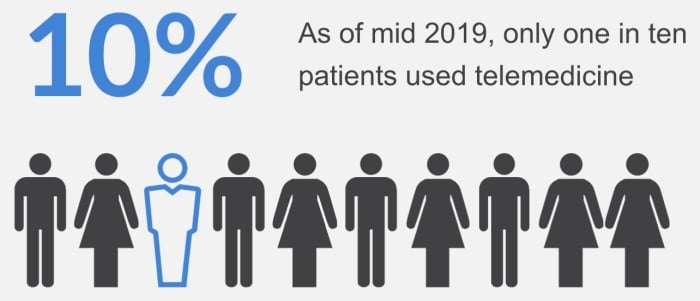
According to a survey by J.D. Power as of July 2019, only one in ten patients used telemedicine services. Today, they have to wait in line on a telemedicine app for hours before they can speak with a healthcare provider.
#6: Better chronic care management with telemedicine
#7: Convenience & improved patient engagement
#8: This billing code turns telemedicine into a revenue source
#9: Telemedicine aligns value-based care with worldwide healthcare objectives
#10: What are the common challenges when using telemedicine?
#11: Telemedicine time
And even though no official data has been shared on the current use of telemedicine, telehealth companies like Amwell are reporting up to 250% – 700% increase in patient visits in different states. Other surveys stress the shift in outpatient visits taking place via telemedicine apps, with 70-76% of all visits becoming virtual vs. 1-3% before the outbreak.
1. Examples of telemedicine
Telemedicine includes many subdisciplines, like teledermatology, teledentistry, teleneurology, telepsychiatry and telenursing. Yet, regardless of the specific area of application, the premise is patients, doctors, and other medical personnel use software (and sometimes hardware sensors) to administer and receive health care remotely.
One popular opinion is that telemedicine has only to do with live video and audio consultations. And while this type of communication is predominant, patients and medical staff also get to interact asynchronously. That second variant is dubbed asynchronous because patients and doctors access and reply messages (text, audio, or video) at their own convenience.
Related: How to Build a Video Chat App
As a broader term, telemedicine may sometimes include remote patient monitoring applications that do not always include audio or video interactivity and instead rely on text messaging. Remote patient monitoring apps typically send patients’ health data to providers in real time, allowing them to assess a patient’s condition.
2. Who can practice telemedicine?
During the COVID-19 pandemic, many states have lifted the barriers for delivering care over the state’s border for all properly licensed healthcare providers. So any doctor that is licensed to serve in a particular state can also assist with delivering care in other states by using telemedicine software.
In addition to removing cross-states care delivery limits, the government has waived HIPAA compliance regulations for the time of the pandemic. This means that doctors can practice medicine with consumer-grade applications like WhatsApp, FaceTime, or Skype. At the same time, it’s worth noting that the HIPAA waiver is a temporary measure and is not a sustainable solution for telemedicine services in the long term.
Some of the medical specialties that use telemedicine the most include:
- dermatologists
- psychiatrists
- neurologist
- cardiologists
- allergists/immunologists
- gastroenterologists
- Ob-gyne
 3. What does telemedicine treat?
3. What does telemedicine treat?
Research has shown telemedicine’s efficiency in many medical fields: from primary care to behavioral health to emergency care when a remote specialist assists local physicians. A teledermatologist can evaluate a patient’s skin condition, a teleneurologist can oversee a patient with Alzheimer’s, a telepsychiatrist can provide consultation to a patient with panic attacks, and the list goes on and on to include nearly all medical disciplines.
4. The benefits of telemedicine and how it is bringing a quiet revolution to value-based care
While some disruptive technologies get a disproportionate share of attention, those that quietly reduce friction and cut costs are often just as impactful, but without making such a splash.
The use of telemedicine to connect patients and physicians has been quietly increasing in medical practice for the last decade. Remote healthcare access has been improving care delivery for all of its stakeholders.
The deployment of connected devices and mHealth is a mobile health revolution. Telemedicine has been evolving as mobile technology has grown. Now, as Centers for Medicare and Medicaid Services has shifted emphasis to value-based care, Medicare providers have an additional incentive to adopt telehealth.
a. Enabling remote care with mHealth
The spread of mHealth applications has made reaching for a smartphone to talk to a doctor an everyday experience. There is a growing library of smartphone and tablet applications that measure physiological conditions and send readings directly to clinics. Doctors can use consumer technologies such as digital tablets and webcams to meet with faraway patients and assess the signals that they previously could only evaluate through in-person encounters.
The quiet revolution has benefited patients in rural communities most where specialized care would otherwise mean travel hundreds of miles. Even patients who do not have access at home can visit local clinics to connect with their specialists online.
 b. Better chronic care management with telemedicine
b. Better chronic care management with telemedicine
Patients that suffer from chronic illnesses, who would otherwise struggle to access to affordable medical care, have a better option and experiences with telemedicine. The Centers for Disease Control asserts that half of the adults in the US have at least one chronic condition and seventy percent of deaths are the result of chronic diseases.
CMS is working to reduce the burdens on physicians when they deliver healthcare services remotely. The agency is extending the number of billable Medicare services and cutting the red tape that healthcare organizations face. Part of that change includes encouraging providers to use enabling technology such as electronic health records and telemedicine.
Related: Healthcare App Development Trends to Watch in 2019
c. Convenience & improved patient engagement
Apart from apparent accessibility and cost benefits of telemedicine, it also improves overall patients’ engagement. They no longer have to wait in the waiting room (the current pandemic aside) and risk catching flu or other diseases from visitors.
Besides, they no longer need to travel long distances to see specialists that may not be available at their local place. Their treatment plan is always accessible via a patient portal, and following up with a doctor is as easy as sending an instant message. Telemedicine enables providers to become more productive and patients more engaged.
d. This billing code turns telemedicine into a revenue source
CMS now provides payment for chronic care management as part of primary care under CPT 99490. This code specifies the use of EHR and, without saying it outright, makes telemedicine a viable channel by which to deliver care within the rules and maximize the revenue that your organization can earn in any given period.
CPT 99490 requires that providers deliver non-face-to-face care for a minimum of 20 minutes per patient per month. In return, they receive a $40 payment. Realistically, the only method to fulfill that requirement and deliver high-quality care is with telemedicine. The code has several additional criteria: Patients must have 24/7 access to their care management services, continuity with a designated practitioner, oversight of medication self-management, among others.
Billing Medicare under CPT 99490 could produce additional revenue of more than $250,000 for per physician each year.
By promoting telemedicine in service to Medicare, CMS is reinforcing the adoption of it for everyone. Providing telemedicine services is one channel across which healthcare organizations can improve efficiency and reach a broader community of patients.
COVID-19 update. The American Medical Association has put together a list of telehealth services covered by Medicare and included in the CPT code set.
e. Telemedicine aligns value-based care with worldwide healthcare objectives
Globally, telemedicine has the potential to do well on a scale that is difficult to estimate. The technology provides support for the Triple Aim advanced by the Institute for Healthcare Improvement: Improve the experience for patients who receive care, improve the health of populations, and reduced per capita cost for care.
There are tremendous benefits to gain from delivering services remotely. The new payment code for US Medicare healthcare providers will help to stabilize the rollout of telemedicine in practice. The change furthers the CMS goal of delivering value-based care to patients and aligns with the Triple Aim of the IHI.
The additional income from qualifying Medicare patients provides the incentive and the sponsorship to make telemedicine part of general practice medical care. The quiet rollout of telemedicine in healthcare practice is bringing to benefit everyone: providers, patients, and the payers too.
5. What are the common challenges when using telemedicine?
The most common types of telehealth challenges include:
- privacy and security issues
- digital divide
- insufficient awareness about insurance coverage
- care continuity concerns
Let’s go through each of these challenges, one by one.
Is telemedicine safe? Depending on who develops your telemedicine solution and whether they follow the industry standards and best practices, such as HIPAA and GDPR, your telehealth app will be a success or flop. We stick to the following cybersecurity standards to protect PHI and patients’ privacy: HIPAA, IEC 62304, ISO27001, SOC2 Type 2, MFi, HITECH Act, GDPR, and a couple of other standards and regulations.
Can all patients comfortably use an iPhone telepsychiatry app? The digital divide still remains a major barrier, with many senior patients not being comfortable using modern telemedicine software. At Topflight, we address that by developing and verifying through user testing patient-centered solutions that work the way people expect them to.
Read about our experience in developing senior care apps.
Does Medicare cover telemedicine services? With the COVID-19 havoc unleashed, many telehealth providers and patients found themselves scrambling to understand insurance coverage policies for telemedicine. To answer this particular question, Medicare will temporarily reimburse the provision of telemedicine services across the entire country. Private payers have followed with similar policies, but the rules differ from state to state.
Will I see the same doctor during a telehealth visit? That’s another question that many patients ask. Indeed, telemedicine does favor the on-demand nature of teleconsultations over consistent e-visits with one and the same specialist. To be fair, this condition has practically nothing to do with the telemedicine technology itself and instead reflects a clinic’s policy.
Telemedicine time
Telemedicine is a booming market. It’s forecasted to reach 175.5 Billion (USD) by 2026. And despite all the challenges, it’s a worthwhile investment option. Schedule a call with us to take your first step towards healthcare app development and learn how your medical practice can best apply telemedicine.
Related Articles:
- Complete Guide to Developing a Healthcare App
- How to create and build a healthcare startup
- Chatbots in healthcare: Use Cases, Best Practices and More
- Patient Portal App Development Guide
- How to Build a Doctor’s Appointment Application
- Guide to building a HIPAA compliant application
- HIPAA Compliant Video Conferencing Application Development
- How to create a pharmacy application
 3. What does telemedicine treat?
3. What does telemedicine treat? b. Better chronic care management with telemedicine
b. Better chronic care management with telemedicine